Editor’s Note: This text is a written transcript of the course, The Role of the Speech-Language Pathologist in the Healthcare Triple Aim, presented by Katie Holterman, MS, CCC-SLP, BCS-S.
Learning Outcomes
After this course, readers will be able to:
- Define the 3 components of the "triple aim" for healthcare.
- Describe how the use of patient self-report, the ASHA NOMS, and other outcome measurements can contribute to the triple aim.
- List at least 2 areas of focus that enable speech-language pathologists to participate in improving the health of the overall population.
- Describe the connection between patient satisfaction and quality of care to reimbursement.
Introduction
I'm really excited to talk about a topic that most people ask what the Triple Aim is and how does it apply to us? A friend actually asked why I like to speak on such a boring topic and that stuck with me. Why do we think it is boring? We are very tuned into our graduate curricula and continuing education that focuses on clinical topics such as how to treat a patient, how to diagnose a patient, how do we get to the crux of the intervention. But, it’s also important to know the other side of things such as how do we impact healthcare and that is what this course will cover.
The Changing Shift from Volume to Value
We have all heard a lot about this changing shift from volume to value. What does it mean to move from volume to value? The problem with hearing this over and over again is that we don't see the immediate results. We slowly approach this shift as an industry, it's not this sudden shift from collecting payment for the volume of services we provide today to moving to a whole new system tomorrow. For those of you working in the SNF industry, there was this sudden shift with PDPM being implemented October 1st. One day we're implementing one reimbursement model and the next day we're not. That's part of this changing landscape. And I think that we hear so often, this shift from volume to value, and it becomes kind of this noise in our head. So, what does this shift from volume to value mean if you are working in healthcare? The Triple Aim is a big part of that shift and comprises so many components of it. While we want to “be over with already” so we can move into this new era, the transition takes a long time and we really need to understand it.
Under the fee for service model, we provide a service, we bill for that service, and we collect for that service. It seemed to be very simple. We are now moving toward a pay for performance model. What does that mean? How do we demonstrate what we do and the value involved in it? I don't know about you, but I am pretty sure that in all of my years of experience and doing what I do, I've never ended the day and said, you know, I gave every one of my patients really bad quality care today. I didn't do anything well. I didn't treat one patient the way they should have been treated. No one does that because we always give our all. We always try to demonstrate the value of what we do and we always try to make the patient better. It's why we got into what we do. Our patients make great results, and that's a great thing. But how do we demonstrate that beyond the clinic, beyond the patient relationship and beyond what we are doing? How do we measure it?
Let’s say you have a patient that comes in to see you for an assessment. You do an extensive evaluation and it takes a long time. Then, you may reassess after seeing them for intervention. Maybe you did a modified barium swallow in the beginning of therapy and a modified barium swallow at the end to show that the patient has good outcomes. Does it stop there? Are we the only ones that know that? How are we demonstrating what we are doing and does it have an impact in the greater picture of health care?
The point is that we need to move out of the silo of speech-language pathology and our own little realm of what we're doing. This is not suggesting that our impact isn't valuable to the patients that we serve, but we have to be able to prove our value in the greater picture. The way that we do this is through contributing to our settings quality outcomes and our care models that we participate in, and becoming a partner in healthcare within our setting.
Triple Aim
The Triple Aim was initially introduced in 2007 and is a framework that was developed by the Institute for Healthcare Improvement in Cambridge, Massachusetts. It has been referred to in a number of different ways. Most of the time, it is called the Triple Aim. Some people call it the Triple Aim initiative, the Triple Aim framework, etc.
There are different terminologies that have been extracted and incorrectly modified from the Triple Aim initiative, and patient satisfaction is a big one. Part of the Triple Aim is patient experience, but that is not the same as patient satisfaction. Patient experience includes safe, effective, patient-centered, timely, efficient and equitable care. You might hear about “reducing costs”. The Triple aim intended to reduced costs on a per capita basis.
The Triple Aim is not aimed at any specific population or age group. It applies to patients of all ages and all healthcare settings, so no matter where you are in the healthcare continuum or who you treat, the Triple Aim has an impact.
The three goals of the Triple Aim are to improve population health, improve quality of care and the patient experience which includes patient satisfaction, and reduce costs on a per capita basis.
The below figure from the Institute for Healthcare Improvement depicts how the Triple Aim is not a type of progression where one thing has to happen before the next thing happens. Rather, it is an overlap.

Figure 1. Overview of the IHI triple aim.
Looking at the graphic, the dot in the middle of the triangle represents the patient. Improving population health, improving the experience of care for the patient, and reducing the cost are on the corners. The idea is that the patient is at the center of everything you're thinking about for these three different components. We can reduce health care costs while we improve quality of care, and as a result, we will improve population health. Likewise, by improving population health and improving the experience, you're going to reduce costs. Again, it is an overlapping feature and that's important to remember.
Improving Population Health
What is population health? It's the health outcomes of a group of individuals, including the distribution of such outcomes within the group. I will explain in greater detail shortly. Population health is different than public health. Public health is the science of protecting and improving the health of people in their communities. You promote healthy lifestyles, research disease and work on preventing infectious disease. Prevention does have a role in population health, but the two are not similar. A lot of people say population health is improving the health of the population by preventing disease. Well, yes and no. Preventing disease is part of it, but it’s not the main part or the only goal. Population health is really concerned with how we are measuring the health outcomes and the patterns of factors that come into play with the health of a population.
There are many factors involved in improving population health. This includes electronic health records, clinical pathways, care models, quality measures. Population health really encompasses what we do for the patient and how we improve their health. That's kind of the mantra I want you to think about: What are we doing to the patient, how are we improving it and how are we measuring it?
Improving Patient Experience
The Triple Aim also focuses on improving patient experience. This is not just satisfaction - satisfaction is a component of it - but also the use of electronic health records, the use of implementing care models. Are we doing patient-centered care? Are we implementing patient-centered care in our goal setting? With patient satisfaction we're looking at outcomes with patient experience as well as patient-reported outcomes and patient-reported satisfaction.
So where does speech-language pathology fit into the Triple Aim? The definition of the Triple Aim is a bit confusing. When I first heard it, I knew that it was initiative in the hospital in which I worked within the context of a rehab department meeting with PT, OT and speech. During that meeting there was a lot of talk about outcome measures for PT and OT. They were discussing improving population health, they were talking about prevention, screenings, and pre-surgery classes for joint replacements. I tuned out because it didn’t seem to involve speech-language pathology. It wasn't until I started to think outside the box that I realized that SLPs have a big part in this initiative. I would like you to think about where you can fit this into your own setting.
Improving Population Health
Let’s start with improving population health. Again, population health is dealing with the overall improvement of the health of the population. How are we improving the population, what are we doing to improve that, what are our outcomes, what are our interventions? Prevention is an important piece. It is a public health component, but it is part of population health.
Speech pathology interventions are thought of as reactive versus proactive. For example, a patient has a stroke, and as a result they have a swallowing issue, they have aphasia, etc. We go in and remediate. We're not proactively going to do aphasia therapy for somebody who might not need it. It's a reactive mode. But where we can be more proactive is by advocating and promoting the profession. We can explain to patients how we can help with early intervention and identify an issue early on.
Screenings are a great way to do this. They can help prevent or even catch potential impairments. One area that we've worked on in some of my former settings is the early identification of vocal nodules. Not only were we educating the consumer, physicians and families about risk factors, but we were also identifying signs and symptoms early on. Dysphagia is another example. We can identify signs and symptoms early.
There's a lot of research on the impact of early intervention that be can be applied to speech-language pathology. More research needs to be done, but in rehab in general, there is a lot of research showing the earlier we rehabilitate, the better the outcome.
Promotion and advocacy of the profession is important. If we're improving the health of our patients, we have to be in it to win it. What I mean by that is if we want patients to advocate for themselves, we have to advocate for them first. We need physicians and other professionals to recognize the value of speech-language pathology services.
Here is an example. I had a patient who had Parkinson’s disease and was having a very difficult time swallowing, was very quiet, and very disarthric. The first time I saw him I asked what interventions he had done so far. He said that he did LSVT BIG for two years. Unfortunately, the physician and patient didn't know that the LSVT LOUD would have helped him. So, that patient outcome could have been improved had we gotten in there a lot sooner. Again, promotion and advocacy of the profession is really important when it comes to the Triple Aim.
Prehabilitation
Prehabilitation is defined as a physical or lifestyle prep that happens before surgery. Really, it can be before any treatment intervention if you consider radiation treatment or those types of procedures. Prehab has a big role in that and is designed to help patients regain function in less time.
Some areas in which prehab would come into play include medical optimization of pre-existing conditions. There's a lot of talk of prehabilitation in the management of patients with diabetes. Optimizing the medical treatment for diabetes prior to any kind of surgery or intervention lessens the chance of infections, post-op infections, etc. Think about our role with a patient who has reflux. There are some complications that come into play with reflux if they're not taking their medications appropriately prior to surgery. We can also have a direct impact if we work with a dietitian. We need to identify any medical condition that we can have a role in prior to the patient going into either a surgery or a procedure.
- Physical fitness - the more fit the patient is, the better the recovery. We want to make sure we are making appropriate referrals for PT, if a patient is already receiving it.
- Nutritional status – this is very important. Think of our patients who are on modified diets, like puree, and may need to go in for surgery. If they have poor nutritional status, it increases the likelihood that they will have a slower recovery. We need to think about how we can participate in the health of a patient and the outcome of a patient given their nutritional status. Are we working with the dietitian? Are we educating the patient? Are we encouraging them get enough hydration? Are we monitoring their nutritional status if they're on any kind of modified diets? We have a role with that and we need to make sure that we're taking an active role in it.
- Psychological support - this comprises patients' cognitive and mental health prior to surgery, motivation and family support. I've had a couple of instances in my career where I've seen a patient post-hip fracture. This is an otherwise healthy patient, but they come in with a hip fracture, they have surgery, and suddenly everything falls apart. They're cognitively out of it. Their swallowing may be impaired. They're having all kinds of speech issues, and we're thinking, “How did this happen with a hip fracture?” How many of those patients had an underlying dementia or had an underlying cognitive decline that was occurring prior to surgery and the effects of anesthesia kind of perpetuated that? Now there's a delirium associated with it and it's not necessarily that we would go in and intervene afterward for that specific dementia because most of the time the delirium will make it clear. But, perhaps we go in prior to the surgery and identify if there is an issue. How often are we going in and have the opportunity to do a baseline cognitive assessment? I realize that is not always easy to implement on a daily basis. But we can ask ourselves how can we try to put this into practice. What can we do to talk with our care teams about how to approach those patients?
Developing Clinical Pathways
Along with improving population health is the development of clinical pathways, which is also very important. Why would we develop these? Developing and implementing clinical pathways streamline the delivery of quality care in the most cost-effective manner. Anytime you can streamline something it makes it easier for everyone involved. Obviously doing something in a cost-effective manner is beneficial. It benefits the patient because they're getting the most standardized treatment by implementing a clinical pathway. They are getting standardized treatment that is hopefully evidence-based. The families have the adequate support. Continuum care partners know that they are working in a team. They are able to follow that pathway so that they know where the patient is in their continuum of care and how that patient is transitioning from setting to setting.
What are clinical pathways comprised of? A clinical pathway is usually comprised of a diagnosis or a group of diagnoses, and it follows the patient diagnosis on how the treatment would be delivered, the assessment, the treatment along all of the touchpoints, all of the disciplines working together.
Basically, all settings can develop and implement clinical pathways. There are barriers, of course, but it can be done. For example, if you are treating a patient with head and neck cancer and you are following the clinical pathways that have been developed, then everyone is on the same page no matter the setting that everyone works in.
Their approach may be a little different depending on the setting, but everybody would have kind of a heart in the game, and it provides the best care for the patient. In some settings, it might be more difficult to develop the clinical pathways based on the diagnosis. For example, if you're in acute care, you may have a pretty solid clinical pathway developed for stroke because that's been really researched. However, you may not have a clinical pathway for head and neck cancer if you setting is not an oncology-based cancer center. Again, it depends a little bit on your setting, but you have to look at what you can do to participate in the development of the clinical pathways. Work with your administration and your leadership to determine how you can be a part of this puzzle.
Can clinical pathways have an effect on cost? Absolutely. By developing clinical pathways, it's been shown that patients have a decreased length of stay in the acute care setting. There's decreased readmission rate, decreased cost and expenses, and decreased labor. There's also a decrease in unnecessary testing. So, there are a lot of effects that developing clinical pathways can have on the cost that you can discuss with your administration when looking at how to develop them.
Clinical Pathways - Examples
Stroke. For many of you, when a patient comes in with a stroke, there's an order set that goes along with that. The patient may have a CT-scan by a certain hour. Referral for speech, referral for PT and OT, referral for social work, and then everybody starts in on what they should be doing. There's a care team that's involved with that. Every intervention should be backed by evidence-based practice or practice guidelines. For example, in my setting, we knew that when developing stroke order sets doing a CT-scan in a certain amount of time was going to improve outcomes. That was backed by evidence-based practice.
Critical care management. This is an area where there is either not a lot of clinical pathways that have been developed or we are not in that piece of the puzzle. However, we should be. There are so many avenues for developing clinical pathways for the different diagnoses that we see in critical care and speech-language pathology having a role in the early ICU involvement can really have a great impact on the patient.
From a communication standpoint, think about early ICU involvement for a patient who's intubated or has a trach. There are unnecessary costs involved in prolonging the length of intubation because the patient can't communicate as well as they need to or may not have a means of communication if they are newly trached. If we're not involved early on, there’s a delay in care that people don't realize we can potentially reduce or control.
Think about being a part of the respiratory team and early improvement of a cough response. How important is that in the ICU and how many times do the critical care personnel realize that we can have an impact on that working together with our respiratory teams? The same is true with swallowing. Obviously, we get in there as early as we can, but, how often is there a fear of aspiration within the nursing staff? We want to educate the nursing care team to recognize signs and symptoms and not being so fearful so that we can improve the patient outcome.
Again, getting in there early, developing those pathways for each of those diagnoses, and keeping in mind all of those areas in which we can work will have a great impact on the patient and the patient outcomes.
Outcomes/Quality
Patient-Centered Outcomes
Examples of patient-centered outcomes include quality of life surveys such as the Voice Handicap Index (VHI), Dysphagia QOL surveys, and the ASHA Quality of Communication Life Scale.
There are also clinician-based outcome measurements. How well did the patient do based on the assessments that you've done? Also, how well is the patient doing in their own quality of life? How are they feeling and how are they thinking that they do? This is part of that patient experience and patient satisfaction that we discussed earlier. But we need to measure not only from our standpoint of think that this patient improved. The patient also needs to think that they improved. Therefore, moving towards patient-centered care by using quality of life surveys is so important. Then we we need to include those results in our goals. That is where we tend to drop off. We may administer these quality of life surveys to some patients, but if we’re not including those results in the patient goals then it’s not really working. And remember, your goal may be different than the patient’s goals. Patient-centered outcomes are just as important as our outcomes.
Specific clinician-based outcome measurement tools include standardized tests and ASHA's National Outcome Measurement System, or the NOMS system, that is made up from the use of functional communication measures. It's a seven-point rating scale and it's clinician-reported. The clinician reports at both admission and discharge. It is free to ASHA members on their website. The data is reported to the national registry at ASHA. There are trends that are collected and reported on, such as different demographics and intervention patterns. It's a great way to have a national comparison of how your interventions are working in comparison to national average, and it's the best way to compare apples to apples in a disciplined, specific way. Again, that is a good way to measure from an SLP standpoint for the outcomes and quality.
Moving Out of the Silo and Finding Our Fit
How do we move out of the silo and find our fit in the greater picture? This is where some of these hospital performance metrics quality measures are going to come in. Some examples include re-hospitalization rates, length of stay, mortality rates and CMS program performance.
The CMS website lists all of the quality initiatives and patient assessment instruments that are used. There's so much involved in quality reporting from a CMS governed standpoint. We don’t have time to go into it today, but it's really important to have a basic knowledge foundation of what these quality performance measures are. Ask questions in your setting about what they are we participating in? How are they being measured? What are we doing with these quality measures? Ask your skilled nursing facility how to be a part of it.
Re-hospitalization
If you ask your facility how measuring re-hospitalization is being measured and how speech pathology fits in, they may say it doesn’t. But this is an opportunity for you to say that we actually do.
Re-hospitalization is a quality measure that looks at the rate that a patient is hospitalized for the same condition within a 30-day timeframe. A key part that impacts not having re-hospitalizations is discharge planning. Discharge planning is not just social work and care coordinators, although they're an integral part of the overall discharge planning process, but we can't forget our role here. How many times have you had the experience, if you're in an acute care setting, where you get a call from the skilled nursing and they say I never got your speech notes. Or, you're in a skilled nursing setting, outpatient, or home health and you don't have the speech notes from acute care.
That transition, that care coordination, is so important because if you decide to proceed without having any of that information, you're putting the patient at risk for a number of things. If you're treating a disorder or issue but you're not sure what happened in the prior setting, then you're going in blind. You have to be part of coordinating that care by coaching, educating, supporting the patient for self-management.
Discharge planning. If we're discharging a patient to home who is on a puree diet or honey thick liquid, and we simply send them on their way, how many of those patients may be re-hospitalized? If they were hospitalized in the first place for aspiration pneumonia, and we're not giving them the adequate education before they go home, they’re going to be re-hospitalized for aspiration pneumonia. So, we have a huge role in being a key part of the education team.
Health literacy. How often are our patients understanding what's important in their health and their medication management, the instructions, the discharge instructions that they have. As communication experts, we must ensure that patients have an understanding of all of the discharge instructions. I don't think that our care partners see us that way. We need to advocate that, as communication specialists, we have a role in ensuring the health literacy of our patients.
Dysphagia. We talked about dysphagia preparedness, modified diets and an education plan for continued care.
Plan for continued care. Make sure the patient knows what's going to happen, where they're going to go and what their follow-up plan is. Do they need additional services? Do they need speech-language pathology services in the home care setting? If they're receiving home care, make sure that it's set up for speech, not just PT and OT. By being an advocate for the patient, we can help reduce re-hospitalization. We want to talk to our administration and say, “I'm a valuable part. I can do this.”
Length of Stay
Acute Care Setting
You're measured on how long your length of stay is. The goal is to reduce the length of stay for several reasons. A major reason is to reduce infection. Research has shown that the less time you're in the hospital, the less of a risk there is for infection.
Early intervention services help reduce the length of stay and we can reduce the length of stay by cutting down on delays along the clinical pathway. How many times do we see delays in radiology? What can we do to improve that and ensure that the patient is moving toward the outcomes in a faster fashion than we are used to?
Subacute - the times are changing with PDPM
We used to have kind of an increased length of stay, and now with PDPM we're seeing a whole shift. If you are working in a skilled nursing environment, we know that there's a variable per diem adjustment now for PT and OT, meaning that there's a decrease in payment after a certain number of days. Speech stays steady, but that doesn't mean that we would keep them forever and ever. CMS is looking at outcomes and how quickly we are able to move patients along the continuum of care. How are we providing treatment? How intensive are our services? If we're only providing services four times a week then maybe five times a week would help the patient move along the continuum faster, more efficiently, and have better outcomes. You can view the quality initiatives on the CMS website (CMS.gov/Medicare/Medicare).
Post-Acute Care Quality Initiatives- IMPACT ACT
Along with the Triple Aim, the Improving Medicare Post-Acute Care Transformation Act, or otherwise known as the IMPACT Act, was implemented in 2014. This is part of the Triple Aim and is working towards standardizing patient assessment data. It's a way to compare apples to apples across the continuum.
There are certain measures in the IMPACT Act that are implemented across all post-acute settings. For example, anybody working in subacute has heard of Section GG. It results in a smoother patient transition between healthcare settings by using the same assessments, same coding systems, and the same language. So, if my patient needed X level of assistance in the skilled nursing environment, that translates to the same language in a home care environment or an LTAH or an IRF. It improves the patient experience by having a universal system to measure across the continuum.
The problem with the IMPACT Act is that the average SLP in a SNF doesn't see the impact and doesn't see where they fit. It's this terminology of what's used as a measurement system for skilled nursing. If you can look at how you would have an impact on all of the measures that are collected for the IMPACT Act, you begin to see that you do have a part in this.
The table below shows the various IMPACT Act domains, what is being measured and which setting is adopting them.
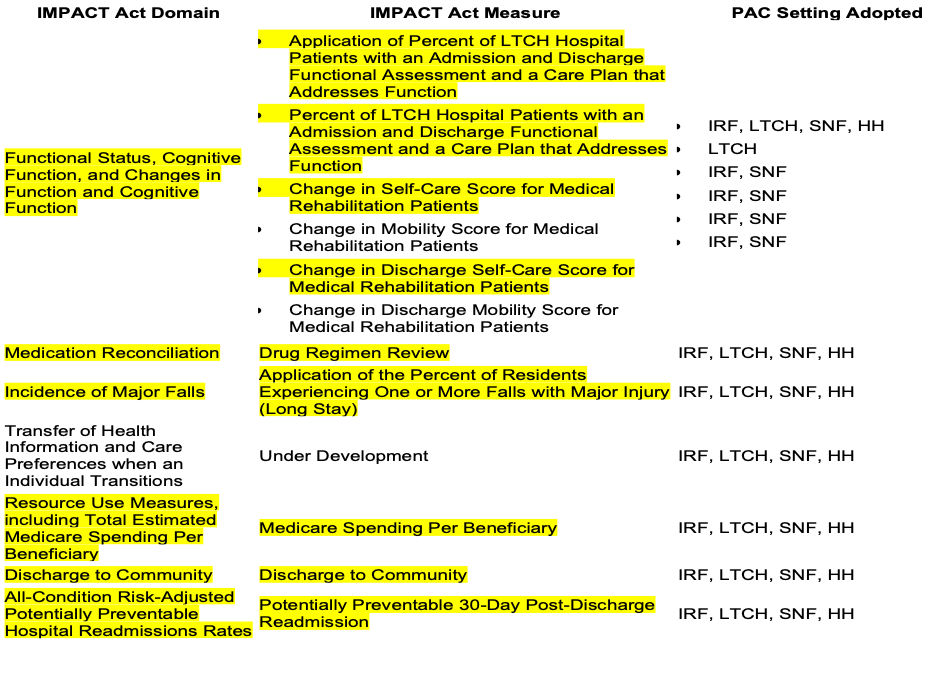
Figure 2. IMPACT Act Domains.
A large portion of what is measured is cognition and we, as SLPs, can definitely have an impact on the patient's cognitive status. We can help identify if there's a cognitive impairment, and how that may impact the patient's score in the assessment.
One of the examples in the table looks at fall rate and the percentage of residents with falls. Most people assume it is due to mobility issues. But what about patients who are confuses or patients who can't sequence appropriately when they're getting in and out of a chair when they're transferring? Again, this is where our role is very important.
Patient Experience
Patient experience is basically the level of satisfaction that the patient felt with the care that they received. Patient experience is not only satisfaction, its quality and determining if the outcomes were met? It's also patient-centered care. Are they engaged? Patient engagement is known to drive toward a complete patient experience. Are they involved in their goal setting? Do they know their expectations? Are we providing adequate education? It encompasses the range of interactions that patients have with the healthcare system which includes ease of appointments and access to their information. Are we using an electronic medical record that allows us to talk amongst systems? Are we providing patient-centered care?
It also involves health insurance. For those working in either private practice or an outpatient setting, are we working with patients to help them understand their own health insurance? And more importantly, do we understand the health insurance? That helps with patient satisfaction and the overall patient experience.
Patient Experience Versus Satisfaction
In order to assess experience, we have to find out whether something that happened in a healthcare setting actually happened or how often it happened. Satisfaction answers the question, “Did we meet the expectations of that health situation?
I want to share a story about “Bert” and “Ernie”, two patients with laryngeal cancer. They both received prehab, had clinical pathways followed, had their pain managed, moved from NPO to mechanical soft, and had support groups. So both patients had the same experience. However, Bert went in non-informed. He learned along the way and didn't know what to expect. Ernie had a good friend who, unfortunately, went through the same thing, so he did know what to expect.
Their experience was the same, but their satisfaction was very different because Bert was not quite satisfied. He didn't know what to expect and he felt confused by the whole situation. Ernie was more prepared, so his satisfaction was different. The point is that we need to know that we're looking at experience and satisfaction in two different ways and we can help navigate along the way by really becoming kind of a captain of that care team and navigating the patient experience in different situations.
How do we measure patient satisfaction? Many of you are probably familiar with satisfaction surveys. They attempt to translate these subjective results into data that's meaningful, quantifiable and actionable. Each satisfaction survey has a direct impact on reimbursement, so we want to make sure that satisfaction is something that we are working on with our patients. What is our role in improving the patient satisfaction of the patient and their family members? How are we communicating that to everyone within our healthcare team?
Reducing Cost
Very simply, we need to have a financial awareness. We cannot be afraid of the “P” word – “productivity”. It's not a negative word. It's not something we love to hear, but productivity does have a time and a place. We need to know what our services cost, and productivity is part of what we cost as a profession. Healthcare is a business, and by having a financial awareness, it elevates us to be able to say, “I need to deliver care in the most efficient and cost-effective way for my patients, not only for the good of the patients, but for the good of the health care system that I'm working for. I need to be working at the top of my license. Am I doing skilled care all the time? Am I reducing non-purposeful care?”
Where's our evidence? Know your evidence-based practice. There's a great campaign called the Choosing Wisely Campaign (choosingwisely.org) which is an initiative of the ABIM Foundation. The mission is to promote conversations between clinicians and patients. It helps patients recognize and choose care that is supported by evidence, not duplicative, and is truly necessary. The AOTA and APTA have taken on this Choosing Wisely campaign and promote it within their profession. I encourage you to move away from tasks like paper and pencil tasks for cognition. Make sure what you are doing is applicable to your patients. but for speech I venture to say, get away from the paper and pencil tasks for cognition. This Choosing Wisely campaign is one where we're advocating for the patient to know what is non-purposeful care? What is evidence-based care? Putting them in the driver's seat.
Reducing Cost - Reduce Unnecessary Spending
Six Sigma Lean is a great way to look at how you can reduce costs. There's a whole program and many hospitals are using it. As I mentioned earlier, reducing cost can happen by starting intervention early on. There is a lot of data to suggest that the earlier we start intervention, the less cost per patient there is. Advocate to your administration that the earlier you get into intervene, the better it is for the patient.
Again, I started with advocacy and I am going to end with it. Advocate for your profession. A higher visibility of services means increased referrals. Higher visibility of services for your consumer means that the patient decides where they're going. The patient decides that they're going to go to hospital A or hospital B. They decide which outpatient setting they're going to go to. They're driving their own health care, and that's part of the Triple Aim in making sure that they are in the driver's seat.
We need to make sure that we're advocating for what we do to help improve patient outcomes. And again, physician education of services is not well known, so talk to your physicians about how speech has an impact in improving the health of the patient, improving the outcomes and reducing the costs associated with disease groups such as, cardiac, pulmonary, neuro, orthopedic.
Here is one last example. I had a patient who had a cervical spine fusion and was having terrible swallowing difficulty. He came in for an MBS. Long story short, the patient’s swallowing was impacted from the surgery. So, I developed a protocol with the referring surgeon to work on prehabbing patients with cervical spine surgeries. If there's any indication of symptoms, we're going to get in early and reduce the amount of complications. We had a subgroup of patients who were having a faster recovery from the surgery overall in comparison to those patients who were not receiving the same pathway. So, it can work and we can have a critical role. We just have to look at where we fit and if we step outside of our box, we can see how we do have a great role in impacting the Triple Aim.
Questions and Answers
Which foundation has the Choosing Wisely campaign?
The website is choosingwisely.org. It is the initiative of the ABIM Foundation, and the AOTA has kind of taken it and moved with it from their professional organization. They've really implemented how to use this campaign for occupational therapy and to advocate for functional therapy. I think cognitive impairment is a good example of how SLPs can look to AOTA and Choosing Wisely and see how we can make therapy more functional.
Do you know if ASHA has any initiatives connected to that? I wonder if this is something that they're talking about.
Not that I'm aware of, but they are looking at more inter-professional practice, and moving towards more functional goals. ASHA is very big on working at the top of our license and so that's part of this as well. Making sure that we are providing only skilled services and functional services and creating goals that are functional.
[Moderator] Good, yeah, I've always found it interesting that when I was practicing clinically, the number and types of referrals I might get varied hugely from facility to facility, so I think there's still a lot of work for us to do as a profession in just promoting our own visibility, like you were talking about, and advocating for what we do and how we do it and our worth and value to perhaps a number of different areas of healthcare, that, I don't know, maybe doctors, nurses, insurance companies don't necessarily think of us as needing to be involved, but where we could play a role, so I really appreciate you being here to talk to us a little bit about that. It's certainly something we should all be keeping in mind in our work settings.
Yes, and if you're not sure where to begin, first you need a foundation of knowing what quality programs are being measured by CMS, by the Joint Commission, by all of these different organizations. You have to know what they are before you know where you can provide value, and so really starting at the beginning is important for everyone.
References
Bakhtiyari J, Sarraf P, Nakhostin-Ansari N, Tafakhori A, Logemann J. Effects of early intervention of swallowing therapy on recovery from dysphagia following stroke. Iran J Neurol. 2015;14(3):119–124.
Cidav Z., Munson J., Estes A., Dawson G., Rogers S., Mandell D. Cost Offset Associated With Early Start Denver Model for Children With Autism (2017) Journal of the American Academy of Child and Adolescent Psychiatry, 56 (9) , pp. 777-78
Golper, L.A.C., & Fratelli, CM (Eds.) (2013). Outcomes in Speech-Language Pathology: Contemporary theories, models and practices (2nd edition). New York, NY: Thieme Medical.
HCAHPS: Patients' Perspectives of Care Survey, Centers for Medicare and Medicaid Services (2020). https:www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-instruments/HospitalQualityInits/HospitalHCAHPS.html
The IHI Triple Aim, Institute for Healthcare Improvement (2020). http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx
Stiefel M, Nolan K. A Guide to Measuring the Triple Aim: Population Health, Experience of Care, and Per Capita Cost. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2012. (Available on www.IHI.org)
Tippett, D.C. 2012. January. Current concepts in treatment planning patient-centered and evidence-based practice in Speech-Language Pathology: SIG 14 Perspectives on Gerontology. Vol 17. 27-33. ASHA
Womack, J.L 2012, April. The relationship between client-centered goals setting and treatment outcomes. SIG 2 Perspectives on Neurophysiology and Neurogenic speech and Language Disorders. Vol 22, 28-35. ASHA.

