Introduction
I am going to spend some time talking about pharmacology and swallowing. I am a speech pathologist in a hospital setting and work in both inpatient and outpatient settings. Those of you who do inpatient hospital or skilled nursing facility work have probably had the same experience as I have, with nurses and physicians asking us, “Is this medication safe to give?” “Can this person swallow it?” “What is the easiest way to swallow it?” “Should we put these medications through the tube?” “Should we crush them?” I had a sense of unease about all of these questions, feeling like I did not really know. I knew a lot about swallowing, but did not really know enough about medications to fully answer these questions that I was being asked. For example, I did not know if a certain medication could be crushed, or should be crushed.
That led to my interest in pharmacology and swallowing. In this course, we are going to try to meet three objectives. I would like you to be able to explain the concepts of pharmacokinetics and pharmacodynamics, as they impact people with swallowing disorders; describe medication effects and side effects and their impact on swallow function; and identify strategies to reduce medication errors for people with dysphagia, because unfortunately, our folks with swallowing disorders are at higher risk for all kinds of medication errors.
There are some handouts for this course that I would like to explain a bit. One is a reference list for all of the studies that I am going to discuss in case you want some additional information. I also put together a medication reference list. As you get started in this area of medication and pharmacology, it is sometimes helpful to have a “cheat sheet” identifying what kinds of medications are anticholinergic, which ones are anticonvulsants, and so on. On that handout, a variety of different medication types are listed along with some of the more commonly prescribed medications that fall into each category.
Overview of Terms and Concepts
Let's begin by defining some terms. There are two aspects - two sides of the coin if you will - to pharmacology: pharmacodynamics and pharmacokinetics. Pharmacodynamics describes how the drug impacts the body; in other words, the therapeutic effects. Pharmacokinetics describes how the body impacts the drug. As we will see, there are implications for people with swallowing disorders in both of these categories.
Pharmacodynamics
If we break this down further and look at pharmacodynamics, we need to talk about the therapeutic effects of the medication. In other words, what the drug is designed to do, whether that is to reduce pain, stop seizures, manage reflux, etc. We have to think about the side effects of the medication, which are many and varied, and that is where many of the dysphagia issues come in. The impact on swallow function is an unintended impact of the medication in most cases, but in fact, it is a side effect that we need to be aware of.
In this area of pharmacodynamics, we also have to think about the site of the activity -- where the drug is actually working within the body. There is a lot of variability. Some medications are very specific in terms of their sites of activity; others are less so, and are therefore more prone to side effects. We will talk about the mechanism of the action as well. How do the drugs work within the body?
Pharmacokinetics
Remember that pharmacokinetics has to do with how the body impacts the drug. There are five different areas: how the drug is administered; how the drug is absorbed within the body; how it is distributed throughout the body; how it is metabolized; and then finally, how it is eliminated from the body. We are going to look at each one of those areas in more detail as we go through the course, and talk about what they mean for our folks with swallowing impairment.
Medications and Aging
We also have to think about our geriatric clients. There are a number of things that change, unfortunately, as we age. Geriatric clients are more likely to have a higher number of medications. They have more illnesses and more comorbidities, so they have more medications on board. Thus, there is a higher likelihood of interactions between those medications.
We also know that swallow function changes as we age, very normally, outside of dysphagia. One of the changes in swallow function is that there is a higher likelihood of esophageal dysmotility. Esophageal clearance and esophageal peristalsis tend to be slower in the aging client. If you already have a baseline slowness in esophageal clearance, that is going to have implications for pill swallowing. It also has implications, then, in terms of any sort of dysphagia that gets overlaid on that.
As we age, we tend to produce less saliva, and so when we talk about side effects, dry mouth comes up quite a bit. If someone is already a geriatric client and their saliva production is somewhat diminished compared to a younger person, and now they are taking these medications that are drying them up even further, you can see how this could cause trouble.
We also see changes, as we age, in liver function, gastric motility, and kidney function. These changes will have an impact on an elderly person's ability to absorb and metabolize medications. Our brain function changes as well; neurotransmitters become less balanced, and that makes us more susceptible to side effects with those medications that have an impact on neural transmission.
So, when we put all of those factors together, as we think about the elderly person on our caseload, we know that person is going to be more drug-sensitive. The therapeutic effects may be exaggerated. They are more prone to side effects. The medications metabolize much more slowly and stay in the system much longer.
There is also a higher risk of drug-induced delirium. We are going to talk about delirium later, but essentially, we are talking about fluctuations in cognitive status. Delirium generally has a fairly rapid onset, so it is different from dementia. It happens very quickly. It is very difficult to diagnose; it is sometimes confused with dementia, or with cognitive changes that occur after stroke. The only way to truly know if this is delirium is to have a good understanding of baseline function so that you are aware of when this is a rapid and significant change from baseline. Elderly folks are more susceptible to delirium. There are many causes of delirium: illness, pain, sleep deprivation, dehydration, or fever. But certainly, the focus of our discussion in this course would be delirium that is drug-induced; that is, the result of either a specific medication that did not get metabolized appropriately or the result of polypharmacy.
Dysphagia
Then, of course, we have to consider individuals who have swallowing impairment, in addition to all of these issues. They are more likely to have difficulty with pill swallowing. That is one of the more challenging swallowing tasks for everybody, even people without swallowing impairments. Certainly, for people who already have some baseline dysphagia, pill swallowing is going to be difficult. We worry about a higher risk of aspiration and a higher choking risk when folks with an underlying swallowing impairment are asked to swallow medications. If a person has a baseline dysphagia, and they are taking medication that has the potential side effect of exacerbating that swallowing impairment, they are going to be more susceptible to those swallow-related side effects. In addition, when we make recommendations for thickened liquids or to take medications in puree, those recommendations have the potential to interfere with how medications are absorbed and metabolized. We are going to look at that in a little bit more detail later.
In the big picture, we have to think about how the medication is impacting the body --the pharmacodynamic piece. We have to think about the impact the body is having on the medication, in metabolizing it, absorbing it, excreting it -- the pharmacokinetic piece. Both of those things are potentially impacted by normal aging - normal changes that happen in the body - and by swallowing impairment. We will examine all of these potential interrelationships (Figure 1) as we go through this process.
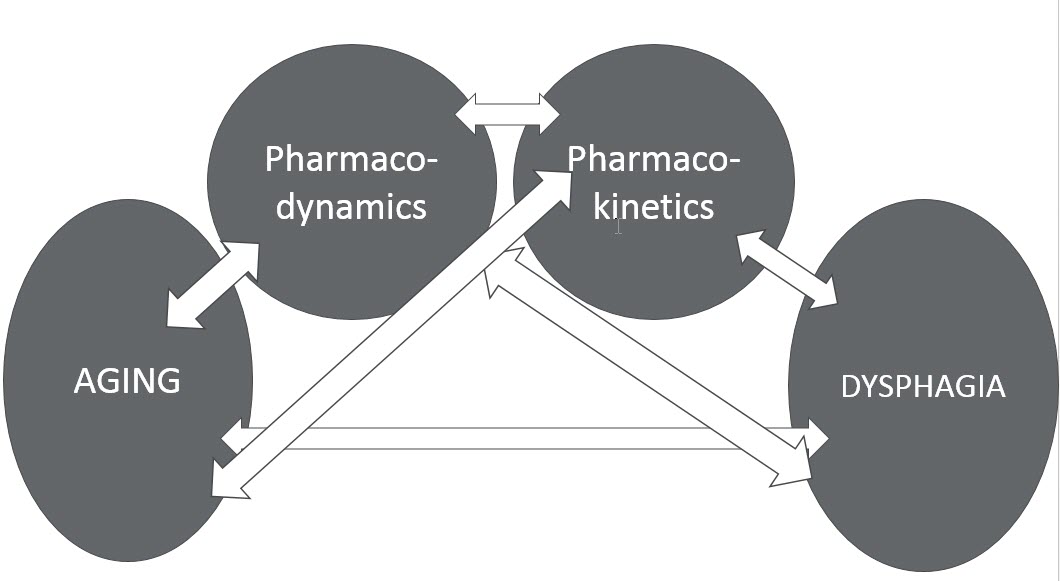
Figure 1. Potential interrelationships.
Pharmacokinetics
Let's start by taking the area of pharmacokinetics and examining it more carefully. There are five areas that we need to look at: administration, absorption, distribution, metabolism and elimination. Just a note, that not all medical sources consider administration - how the drug enters the body - to be part of pharmacokinetics. Some sources do while others feel it is a separate process. But as speech pathologists, how the drug gets in is a big focus of ours, so we certainly are going to spend some time talking about it. Absorption is the process through which the drug moves into and through the bloodstream, and thus into circulation. Distribution is the transportation of that drug to the target site or sites where the drug is going to have its impact. Metabolism is how the drug is chemically altered. The goal of that chemical alteration is the final step in the process, which is excretion or elimination. Eventually, the ultimate goal of the body is to get rid of this drug -- to excrete it.
Administration
Let's start with administration. Administration is the manner by which the drug enters the body and there are any number of ways that this could potentially happen. There are topical medications; for example, creams that are placed on the skin. Some medications are taken sublingually, like nitroglycerin or sometimes Vitamin B12. We have all seen patients who have transdermal medications delivered via patches on their skin. The most common one is the nicotine patch. Some medications are administered rectally, like suppositories for nausea. Some medications are inhaled. Patients who have asthma or chronic obstructive pulmonary disease (COPD) might be taking medications that are administered through inhalation. In acute care settings, we see patients who are receiving medication intravenously (IV), directly into the bloodstream. Medications can also be delivered via subcutaneous administration, just under the epidermal layer of the skin; insulin is a good example of that. Intrathecal administration is administration into the spinal canal. Baclofen is a good example of that. And of course, there is oral administration. That is where we come in, because that is where we are often asked to make recommendations in terms of the easiest and safest way for patients to take their medications by mouth.
The idea of pill swallowing - oral administration - is not so easy. A few studies that were not looking at people with swallowing impairment found that even in the absence of other swallowing problems, anywhere from 10 to 44% of the general population will report difficulty with swallowing pills (Carnaby-Mann et al, 2005; Marquis et al, 2013; Schiele, et al, 2013). In a study with Parkinson's patients, 14% of the patients with Parkinson's disease were having difficulty swallowing their pills (Walker, et al, 2011). The Schiele (2013) study looked at patients who had known swallowing impairment and had mental illness, and those folks were having a lot of difficulty taking their medications by mouth, not surprisingly.
But here is the other part of the problem. We have all these folks with and without medical diagnosis, with and without dysphagia, who are having difficulty with pill swallowing. But 70% of the folks who reported difficulty with pill swallowing also felt their physician probably did not know about their difficulty with pill swallowing (Schiele, 2013). Physicians cannot make accommodations if they do not even know that their patients are having difficulty taking their medication. Marquis et al. (2013) asked respondents if their pharmacist or physician had asked them about difficulty swallowing. As you see, that was not a commonly asked question. So, there is this assumption that everybody is swallowing their pills without any difficulty; but in fact, there are a lot of people who are not swallowing their pills without some degree of difficulty.
If you can’t swallow your pills, if you are anxious about swallowing your pills, if you simply cannot swallow your pills, then you are not going to take your pills. So there is a higher rate of non-adherence to medication regimes. More of these folks are likely to report that they altered the medication in some way -- that they crushed it, or opened the capsule, or cut it in half. Depending on the medication, that may or may not be an appropriate thing to do, as we will see.
Dysphagia and pain medication. Another study was conducted to not only interview the individuals who were having difficulty swallowing, but also the physicians (Pergolizzi, et al, 2014). Over 1000 patients and 30-plus physicians were included in this survey. The physicians estimated that anywhere between 5-20% of their patients were probably having difficulty swallowing medications, but almost 30% of the patients themselves reported that they were having difficulty. The physicians seemed to be underestimating the number of patients who were having these difficulties. Additionally, those folks who were having difficulty reported cutting their pills or crushing them in order to take them, but the majority of them did not know that by doing that, they were potentially altering how the medication was released. We clearly have a knowledge gap here. Physicians are not always aware that their patients are having difficulty swallowing the medications. The patients are not talking to their physicians or pharmacists about it, and are altering medications in ways that may not be appropriate, given the type of medication that they are taking.
Tablet/pill swallowing. What about the actual swallow physiology? What is involved in terms of pill swallowing? It turns out that swallowing pills is different than swallowing food and different from swallowing liquid. In Yamamoto et al.’s (2013) study, they were looking at individuals with normal baseline swallow function; these were not people with dysphagia. The researchers had them do pill swallowing with liquid to see the impact on swallow physiology. There was a tendency toward more oral retention, and a tendency toward more muscular activity. Thus, we are working a little harder when we have to swallow these more challenging boluses.
There were also differences with different types of pills. Medications that were not coated or medications that were a little larger resulted in more muscular activity. Depending on the medication formulation, we may have to work a little harder in order to swallow them efficiently.
Of course, we have concerns about people who already have swallowing difficulties, who are now asked to swallow these more challenging boluses. Kelly et al. (2009) asked people with dysphagia to swallow different types of medications, to see what they felt was easier. There was no imaging used; this was just the patient's perception of what was easier and what was harder to swallow. Not surprisingly, coated tablets were reportedly easier to swallow. Capsules or torpedo-shaped drugs were easier to swallow than round tablets, which might be a little surprising. Smaller pills were generally easier than larger pills to swallow. And once again, these folks reported that their pharmacists did not know they were having any difficulty.

