Editor's note: This text-based course is a transcript of the webinar, Covid-19 With Older Adults: An Update, presented by Krista Covell-Pierson, OTR/L, BCB-PMD.
Learning Outcomes
- After this course, participants will be able to identify COVID-19 information and resources to implement this into treatment plans with patients and families.
- After this course, participants will be able to list effective infection management strategies.
- After this course, participants will be able to list occupations and mental health issues related to COVID-19.
Introduction
Therapy professionals have a role in older adults' lives amidst COVID-19 because we address activities of daily living (ADLs), safety, quality of life, mental health, and other directly impacted areas. Depending on our work setting, this experience has affected us all differently.
When COVID-19 first hit, I was fearful for my clientele as they were at high risk and often alone. I also feared for my colleagues. Many things have changed like immunizations, boosters, treatment protocols, guidelines, etc., but we are entering year 3 of the global pandemic. There is still a lot of uncertainty and unknown. And, we all have stories of how this has affected us. Figure 1 is an image of me with a patient pre-COVID.

Figure 1. Krista with a client before COVID-19.
Figure 2 is an image of Krista after COVID-19.

Figure 2. Krista after Covid-19.
We all miss the things we were able to do in the past, such as smiling at our patients without a mask, and it has been a process to feel like we can provide quality care. No one is an expert in COVID-19, but we all do our best with the information we have.
Our World Now
The older adult population has been significantly impacted by COVID-19. According to the Centers for Disease Control and Prevention (CDC), more people have died from COVID over 65 than any other age. Here are two links that track data.
COVID-19 Weekly Deaths per 100,000 Population by Age Group, United States
Individuals often cannot have visitors when hospitalized for this disease, depending on location and hospital policies. I had a family member in the hospital early on in the pandemic that was 89 years old, had dementia, and was not allowed any visitors.
In the beginning, nursing homes were a breeding ground for the virus, and older adults were more impacted because they were alone in their homes for days on end. With vaccines and other precautions, less spread is being noted in nursing homes. Here are some critical updates for long-term care on this CDC page:
- Updated outbreak response guidance to promote use of contact tracing approach. Alternative broad-based approaches to outbreak response at a facility-wide or unit level are also described.
- Updated expanded screening testing recommendations for healthcare personnel (HCP).
- Updated recommendations for quarantine of fully vaccinated residents.
- Updated visitation guidance.
Older adults continue to be isolated due to COVID and do not necessarily have the same capabilities that we do with technology. Therapy and other health professionals have a role with this population. As we continue to move through the pandemic, we will need to do our jobs safely and effectively amidst this turbulent time.
Where Does Therapy Fit with COVID-19?
The message to older adults and those with compromised immunity continues to be that staying at home is better causing continued occupational disruption. They have more falls, diminished ADL quality, decreased life satisfaction, and declining mental health and cognition. We are seeing an overall breakdown in people's ability to function at their best. We may not be experts in COVID-19, but we are experts in helping people struggling with their occupations. No matter what setting we work in with older adults, we can help and have an impact.
Things continue to change. We have to discern what is appropriate for our unique circumstances and clientele and use clinical judgment and empathy to promote safety. We may need to make decisions quickly and pivot depending on what is happening with COVID-19. Not everything we talk about today will apply to every person. Wherever you are, I hope you can adapt what we talk about according to your setting.
Older adults can mean anyone from 65 years old to a healthy, vibrant 90-year-old. In fact, I met two seniors in their 80s hiking. When they told me how old they were, I was shocked because I do not typically see older adults at that high level of performance. They are examples of "well elderly," but there can also be a 65-year-old who has Parkinson's and other comorbidities. We work with a range of people, and we have to be creative. As another example, I had a 72-year-old patient with cancer who was a paralegal. I helped her return to work and reduce her potential exposure.
The recovery process from COVID for many of our patients is quite long. Some have come home after hospitalization, but others have been put in a skilled nursing facility or in long-term care. We want to integrate COVID-19 information into treatment plans with patients and families. There is a ton of information about COVID-19 that is constantly being updated, and we must address COVID as part of our patient's occupational profiles. To do that, we must have the appropriate information ourselves and know where to go for that information.
History of Coronavirus
Learning about COVID's background helps us give our patients and their families quality information. It also helps us make decisions and reduce anxiety for ourselves, our patients, and their families. According to the Centers for Disease Control, human coronaviruses were first discovered in domestic poultry in the 1930s and first seen in humans in the 1960s. The word corona means a crown, referring to the crown-like spikes on the surface of the virus.
Types of Coronaviruses
Seven types of coronaviruses can infect people. Four of them are most likely what causes the common cold. The other three types cause severe lung infections, which is what we are seeing presently:
- MERS
- SARS
- COVID
Some of you may have heard of Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). It is believed that MERS, SARS, and our current virus were initially in animals only but then transferred to people.
The initial discovery of COVID was in Wuhan, China. When patients became infected, they had a link to a seafood and animal market, indicating an animal-to-person spreadability. As more people became infected who did not have contact with that market, it became apparent that the virus was now spreading person-to-person. By the middle of May 2020, it was present in 212 countries and all 50 states in the United States. We have never seen that kind of spread, and there is no natural immunity to it. It can cause mild to severe illness. Those over the age of 65 or with underlying health problems are most impacted.
The name of this virus is SARS-CoV-2, and it causes COVID-19. The "19" in COVID-19 refers to the year it was discovered.
Go To Trusted Sources
There is a lot of information circulating about COVID and its variants. If patients and their families have questions about COVID, we have to provide them with good sources:
- The World Health Organization
- Centers for Disease Control and Prevention (CDC)
- Federal Drug Administration
- National Institutes of Health
- Department of Health and Human Services
- State health departments
- City and county health departments
We should not be sharing news that we get from Facebook but instead use reliable organizations. Even though politics are brought into the coronavirus conversation, we should not talk about that with our patients. Instead, we want to refer people to sources like the World Health Organization. The CDC, part of the Department of Health and Human Services, has easy-to-read graphics and information (as noted in the above links). The purpose of the CDC is to protect Americans from health threats both here and abroad. It is essential that your client and their family know where to go for updated information including from state health departments. I live in Northern Colorado near Greeley, an early hotspot. I needed to know what was going on there and in my county. You want to educate your patients and take the time to help them get access to those sources in their areas.
COVID-19 Versus the Flu
Some of our patients still think that COVID and the flu are similar. As a health professional, you have the language and knowledge to talk about the commonalities and the differences. Some of our clients are overwhelmed with new information.
- Commonalities
- Cannot be treated by antibiotics
- Droplet transmission
- Handwashing helps with prevention
- Both respiratory
- Differences
- Spreadability
- Severity
The flu and COVID are caused by viruses that antibiotics cannot treat. The flu is caused by the influenza virus, similar to how the SARS-CoV-2 virus causes COVID-19. Sneezing and coughing release droplets into the air and gets into other people's eyes, noses, and mouths. And, "it may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads" (FAQ: FDA.com). Handwashing helps with prevention.
Spreadability is one of the biggest differences. We know that people can experience symptoms for one to four days after being infected with the flu. It can be spread in the first one or two days before a person realizes they are sick. With COVID, people typically experience symptoms for two to 14 days after being infected (CDC).
- Symptoms
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
"This list does not include all possible symptoms. CDC will continue to update this list as we learn more about COVID-19. Older adults and people who have severe underlying medical conditions like heart or lung disease or diabetes seem to be at higher risk for developing more serious complications from COVID-19 illness" (CDC, Feb. 2021).
Given what we currently know about COVID-19 and the Omicron variant, CDC is shortening the recommended time for isolation for the public. People with COVID-19 should isolate for 5 days and if they are asymptomatic or their symptoms are resolving (without fever for 24 hours), follow that by 5 days of wearing a mask when around others to minimize the risk of infecting people they encounter. The change is motivated by science demonstrating that the majority of SARS-CoV-2 transmission occurs early in the course of illness, generally in the 1-2 days prior to onset of symptoms and the 2-3 days after.
Additionally, CDC is updating the recommended quarantine period for anyone in the general public who is exposed to COVID-19. For people who are unvaccinated or are more than six months out from their second mRNA dose (or more than 2 months after the J&J vaccine) and not yet boosted, CDC now recommends quarantine for 5 days followed by strict mask use for an additional 5 days. Alternatively, if a 5-day quarantine is not feasible, it is imperative that an exposed person wear a well-fitting mask at all times when around others for 10 days after exposure. Individuals who have received their booster shot do not need to quarantine following an exposure, but should wear a mask for 10 days after the exposure. For all those exposed, best practice would also include a test for SARS-CoV-2 at day 5 after exposure. If symptoms occur, individuals should immediately quarantine until a negative test confirms symptoms are not attributable to COVID-19.
Goal and Treatment Ideas
I want you to have ideas that you can put right into your care plans. Depending on your setting, you should be screening people for COVID signs and symptoms every day and should be doing temperature checks for yourself as well.
At my company, we request that patients get screened by the therapist and have the therapist screen themselves twice a day. We use a non-contact thermometer that you use by pointing it at your forehead. If somebody spikes a fever, that is our first red flag. If somebody then develops a dry cough or feels tightness in their chest, we should call the healthcare provider. We also provide mobile screenings in people's homes. We screen patients and ask where they have traveled. We then take temperatures and ask about possible signs and symptoms of COVID. If somebody has spiked a fever or shows symptoms, we do not complete the treatment but instead, get in touch with the home care provider.
Your work setting should show you how to screen your patients for COVID, but no matter where you work, you need to ensure that you remain diligent. For example, early on in the pandemic, we had a speech-language pathologist who also worked in a hospital. She went to work and felt fine, but she had a slight fever (under 100.4 degrees) when she was screened at the hospital. Her employer sent her home, and by that evening, she was in the hospital on a ventilator with COVID. She had been in front of other patients for two weeks before that, so everybody had to be contacted. I share that story because it drives home how important this is. We have to keep people safe and do these screenings.
Empower Clients and Families
You should ask your clients about their knowledge of COVID-19 right away and then share information if they are incorrect or are stating something that is no longer true. You may also want to assess where they are getting their information. You can encourage a client to independently locate resources and add that as a goal to your treatment plan. The landscape is ever-changing, and we want to make sure that they know what to do if there are changes in the community. An essential part of discharge planning is understanding where to get updated information. I also recommend creating a handout about infection control, resources, websites, and local organizations.
Use of Personal Protective Equipment
Infection prevention strategies are essential for those working with patients with COVID or who are presumably positive. If they are not getting tested, adherence to your organization's infection control policies is critical. I cannot emphasize enough how important it is for therapists to protect themselves, their families, and their patients.
Here are some points to remember about personal protective equipment (PPE):
- Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must:
- Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE.
- Demonstrate competency in performing appropriate infection control practices and procedures.
- Remember:
- PPE must be donned correctly before entering the patient arena (e.g., isolation room, unit if cohorting).
- PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/ face mask) during patient care.
- PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be developed and used during training and patient care.
You should receive training on infection prevention from your employer. It is essential to know how to put PPE on and take it off. If you do it incorrectly, you can spread the virus. If you feel like you are not getting enough training, I encourage you to look at some resources and take them to your management team. We want to make sure that everyone is getting the support they need. One of our hospitals had registered nurses help the intensive care unit team because they noticed that they were taking off their PPE and storing it incorrectly causing cross-contamination. Speak up if you see something. There should be an infection control person that you can talk to as well. The CDC requires people working with folks who have COVID to have a face mask, goggles, a pair of clean non-surgical gloves, and an isolation gown.
The PPE recommendations are being updated regularly so check frequently.
Donning PPE
More than one donning method may be acceptable. Training and practice using your healthcare facility's procedures are critical. Below is one example of donning:
1. Identify and gather the proper PPE to don. Ensure that the choice of gown size is correct (based on training).
2. Perform hand hygiene using hand sanitizer.
3. Put on an isolation gown. Tie all of the ties on the gown. Assistance may be needed by another HCP.
4. Put on NIOSH-approved N95 filtering facepiece respirator or higher (use a facemask if a respirator is not available). If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented. Do not pinch the nosepiece with one hand. The respirator/face mask should be extended under the chin. Both your mouth and nose should be protected. Do not wear a respirator/face mask under your chin or store in a scrubs' pocket between patients.*
● Respirator: Respirator straps should be placed on the crown of the head (top strap) and the base of the neck (bottom strap). Perform a user seal check each time you put on the respirator.
● Facemask: Mask ties should be secured on the crown of the head (top tie) and the base of the neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
5. Put on a face shield or goggles. Face shields provide full-face coverage. Goggles also provide excellent protection for the eyes but fogging is common.
6. Perform hand hygiene before putting on gloves. Gloves should cover the cuff (wrist) of the gown.
7. HCP may now enter the patient room.
Doffing PPE
More than one doffing method may be acceptable. Training and practice using your healthcare facility's procedure are critical. Below is one example of doffing:
1. Remove the gloves. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
2. Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so in a gentle manner, avoiding a forceful movement. Reach up to the shoulders and carefully pull the gown down and away from the body. Rolling the gown down is an acceptable approach. Dispose of in a trash receptacle.
3. HCP may now exit the patient room.
4. Perform hand hygiene.
5. Remove face shields or goggles. Carefully remove the face shield or goggles by grabbing the strap and pulling upwards and away from the head. Do not touch the front of the face shield or goggles.
6. Remove and discard respirator (or facemask if used instead of respirator). Do not touch the front of the respirator or facemask.
● Respirator: Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
● Facemask: Carefully untie (or unhook from the ears) and pull away from the face without touching the front.
7. Perform hand hygiene after removing the respirator/facemask and before putting it on again if your workplace is practicing reuse.
Figure 3 shows the difference between an N95 respirator mask and a surgical mask:
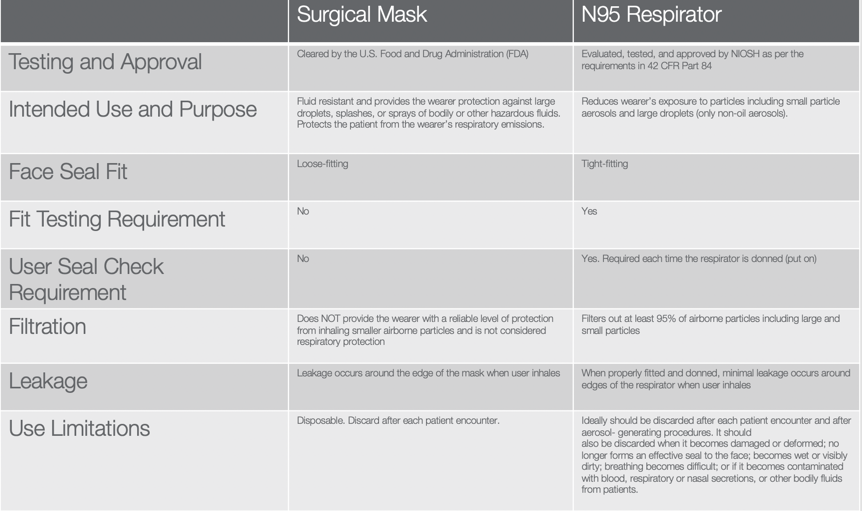
Figure 3. N95 respirator mask vs. surgical mask.
https://www.cdc.gov/niosh/npptl/pdfs/UnderstandDifferenceInfographic-508.pdf
Depending on your work setting, you may be familiar with these routines. However, this is not the case for many therapists. Make sure that you all have good resources and know where to go. It is important to educate yourself in order to feel confident.
Know Your PPE Requirements
Whether or not you see clients with COVID, you need to be educated about putting infection prevention practices in place every day. We have to do our due diligence and follow our local community guidelines when we are away from work. We can also look to our supervisors and local and national organizations for guidance.
Figure 4 is an image of Jessica Shell.

Figure 4. An Image of a staff member with PPE.
It can be exhausting and tiring if you are wearing full PPE like Jessica.
Safety Starts with You
For some, it may only be required to wear a surgical mask seen in Figure 5:
Figure 5. Staff taking safety measures.
These are two talented occupational therapists that I have worked with for the last couple of years. They work with a company called Thrive Therapy and have seen patients throughout the pandemic in an independent assisted and memory care facility.
Handwashing
As healthcare professionals, we understand the importance of handwashing. It is recommended that people wash their hands for 20 seconds or more to be effective. Here is some information on hand sanitizer.
There are important differences between washing hands with soap and water and using hand sanitizer. Soap and water work to remove all types of germs from hands, while sanitizer acts by killing certain germs on the skin. Although alcohol-based hand sanitizers can quickly reduce the number of germs in many situations, they should be used in the right situations. Soap and water are more effective than hand sanitizers at removing certain kinds of germs like norovirus, Cryptosporidium, and Clostridioides difficile, as well as chemicals (CDC).
How Therapy Can Help with PPE with Older Adults
I am now going to discuss developing creative ways to connect with older adult patients despite wearing PPE and practicing social distancing.
Goals for Handwashing
Figure 6 is an image of my patient, Tom.

Figure 6. Incorporating handwashing into treatment.
It is beneficial to set a specific goal related to handwashing. You can include factors like independent initiation if you remind your patient every time. Are they washing them after they do certain tasks or after seeing somebody? You also want to consider how they wash their hands. Do they use soap and water? You then want to talk about how to manage that in public places. These factors can be built into a treatment plan for education and safety.
A goal I recommended for a patient is completing handwashing independently with proper technique, soap, and water, and for 20 seconds or more for three out of three consecutive sessions. The ability to change this patient's handwashing was a challenge, but she was in the early stages of dementia. She was able to integrate some new habits. We also put up a few signs next to her sink to help her remember what she was supposed to do.
Talk with Patients about PPE
Make sure you talk about your PPE with your patient and explain that you wear it for their safety. Emphasize that you work with sick, compromised, or older adults. You can also ask the person to wear a mask.
I can give you the verbiage that I have used. "Before we start our session today, I want to talk with you about how I do infection prevention. I know you are eager to tell me how you have been doing since our last session, but let's make sure we do our supervised handwashing." I then wash my hands in front of them and vice versa. You can also say, "I know you are going out in the community more. Tell me how you manage your mask when you are out and about. Can you show me how you are putting it on and taking it off?"
Hang Up a Picture
We have been displaying pictures of ourselves taken before COVID. These photos can be great for clients to see a natural face. Figure 7 is an image of Rita Stern, a nurse practitioner who I work with:

Figure 7. Krista with a coworker.
She does house calls and sees our patients at some of our facilities. It is excellent for me to say, "I am going to ask that Rita comes in and sees you. Here is a picture of Rita because she will be wearing a mask." You could also put a picture of yourself on your name tag. This can help build human connection despite the PPE in the way.
Get Creative with PPE
Here are some ways you can modify PPE creatively:
- Use masks with "windows" if appropriate
- Reduce background noises
- Modify and adapt patient masks as appropriate
Figure 8 is an image of Amy, who is the speech therapist who tested positive for COVID-19 with a mask with a clear window.

Figure 8. Mask with a clear window.
This picture was taken after her experience with COVID. They are great for therapists who work with clientele that are hard of hearing. When a patient has a low-voice projection, wearing a mask can be tough. Due to this, we want to make sure we are reducing background noises. Improving posture and stretching may also help with hearing loss.
Modifying Masks Video
We have to consider many different things when it comes to masks, and I encourage you to follow CDC recommendations. Putting masks on and off for our older adults is more challenging than expected. This is especially the case for those who have shoulder problems, neck problems, glasses, or hearing aids. This is a video of Gail, who works with me as a personal trainer and works in one of our independent living facilities. She figured this out for her patients in Video1.
As therapists, we can exchange buttons for Velcro and shoelaces for elastic. Again, we need to follow recommendations for current mask use as this area is constantly being updated.
We also teach people how to don/doff different types of clothing. Wearing a mask is now part of that. You want to make sure that they are donning and doffing it appropriately. In a rehabilitation setting, therapists have to think about the next phase for clientele outside of the facility. It could be in their home, the community, a return to work, or assisted living.
I had a patient who started to go back into the community and do his grocery shopping. He had gloves, a mask, and hand sanitizer. However, he took the mask off from the front and put it into the console with his gloves on. This means he was using dirty gloves, putting the mask down, taking the gloves off, and putting the dirty gloves in the console. He then touched the ignition, the steering wheel, and his face. We needed to discuss removing the mask from the straps and when to wash his hands. We have to teach people how to do these things as we learn to do them ourselves.
There are many different ways to put infection prevention into our treatment programs. This will benefit the public, our patients, and their families. We want to empower them because this is the new normal, and it will probably stay this way for a while.
Activity Analysis
This is an excellent example of activity analysis and incorporating infection prevention into your ADLs. If you can go out in the community with your clients, you will learn a lot. Figure 9 shows an example.

Figure 9. This shows an example of an IADL where you could work on infection control.
Goal and Treatment Ideas
We need to bring the COVID impact into evaluations and occupational profiles. Your evaluation forms will most likely not ask how COVID has impacted your patients, especially regarding their ADLs. It is up to practitioners to bring that into documentation, mindset, and plans. It has to be defensible because we help patients stay functional and safe during their ADLs.
Since we work in various settings, not all treatment ideas apply as I explain them. If you are not in an environment that allows for multiple treatment sessions, you can create a handout for your patients and their families to read on their own time. This can include general information, not just COVID precautions and ADLs. Your team can also make informational videos or provide treatment virtually.
For those of you working in skilled nursing, I have always loved working with a restorative nursing program. Now is a great time to revamp your programs because they do not always have to be about exercise. Think about increasing socialization or adding FaceTime to some of the programs. This is an opportunity for creativity. Therapy professionals can become leaders and tie performance with COVID's primary and secondary impacts.
The client's context is being impacted no matter where we are, so we must consider that throughout our treatment sessions.
Positioning
Those of you who have worked with patients with pneumonia or chronic obstructive pulmonary disease (COPD) know that positioning impacts respiratory function. This applies to patients with COVID as well. Putting patients in a prone position on their stomach improves respiratory function and reduces pressure since there is no tissue on the backside of the lungs. When our patients lie on their backs, that creates more pressure through the lungs and makes breathing more difficult. Being prone opens up the diaphragm, the primary muscle used in breathing. Position change can improve recovery time and reduce the severity of COVID symptoms.
Moving patients into this position is not a new tactic. Before ventilators, putting people in a prone position was one of the primary interventions for about 20 years. If somebody is in respiratory distress and is in the ICU, it is recommended that they remain prone for 16 hours a day. That is a long time, and some people cannot tolerate that. Hospitals are integrating programs where people are prone for four hours twice a day. We also need to think about when positioning makes sense. If somebody is in the ICU, it may not be as appropriate, but you can use prone positioning in other settings, such as home care or skilled nursing.
As a therapist, you can come in and assess comfort, skin irritation, and breakdown risk. You can help patients be functional in various positions. If they are lying on their stomach the whole time, can they watch television or listen to books on tape? This can help them enjoy that time and make it go faster. We may have to modify positioning devices as well to keep people safe. If you are working in a setting where you think that might be helpful for patients, I encourage you to talk to your medical team to see if that is something you want to put into place.
Many older adults who get sick do not necessarily go to the hospital or get placed on a ventilator. If we can help them in a prone position during their recovery, this would be an excellent intervention in any setting.
I have an example from a skilled nursing facility in Greeley, that was a hot spot with over 30 percent of their population infected with COVID. Once the occupational and physical therapists started integrating positioning with their COVID patients, they saw that they were not getting sick or staying sick for that long.
The recommendation is to start prone positioning as early as possible. You can educate your patients on prone positioning interventions. This way, if they know somebody that gets sick, they can integrate that themselves.
Activity Engagement Post-Intubation
What happens when we see patients after COVID? This is probably where most of us are seeing our patients. Research says that helping patients move as soon as they are medically cleared can enhance long-term, successful recovery. The recommendation is that a patient is up for about seven days a week. This is difficult if patients do not feel good, and it can be hard to motivate them. However, a therapist can integrate that into their treatment plan and create goals around that. We can monitor their participation, initiation, execution, and how many times they have to take a rest. We can help with that because we are good at assisting people to engage in meaningful activities. We can integrate that with sitting up longer, being on their feet, or getting supplies together.
Promoting Respiratory Health
Many therapists are already integrating respiratory health into their treatment plans. We need to consider doing this more with our older adult patients. Research is mixed on whether or not increasing lung strength helps patients prevent symptoms of COVID-19. I have information from John Hopkins University, and it reads as follows:
In pneumonia, the lungs become filled with fluid and inflamed, leading to breathing difficulties. For some people breathing problems can become severe enough to require treatment at the hospital. At the hospital with oxygen or even a ventilator, pneumonia with COVID-19 tends to take hold in both lungs. Air sacs in the lungs fill with fluid limiting their ability to take in oxygen and causing shortness of breath, cough, and other symptoms. While most people recover from pneumonia without any lasting lung damage, pneumonia associated with COVID-19 may be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.
We can promote diaphragmatic breathing and pursed-lip breathing. If you are not sure how to do that or need practice, there are online resources that can help with that.
I have used breathing strategies in several of my treatment plans over the years for various situations, such as mental health, stress management, community mobility, and increasing activity tolerance. You could write a goal for a patient to complete lung exercises using the Breath Ball app for five to seven days demonstrating a good technique.
Author Tim Winton says, "It's funny, but you never really think much about breathing until it's all you ever think about." Working with people that have COVID, I can relate to this. It is a scary situation with a lot of anxiety and breathing difficulty. If we can educate people on good lung function, how the lungs move, and how the diaphragm interacts, they can stay in control. However, I do not want to confuse this with respiratory distress, which is a medical emergency that they can breathe their way through.
Promote Good Diet and Hydration
On top of the physical exercises that we can do to support patients' lung health, we can also integrate diet and hydration into our treatments. Many therapy professionals leave this aspect to the dietitians. However, if someone is always eating junk food or drinking diet soda, this is not going to support their health and ability to prevent infection. We want to build up people's resiliency and immunity as much as possible.
Proper hydration is vital with lung health because it maintains adequate blood volume and healthy mucous membranes in the respiratory system. If older adult patients have incontinence, they may not want to drink more. You may have to start slowly with your treatment plan. If they only drink eight ounces of water a day, increase that to 16 ounces. You can say, "The next session you should be drinking 16 ounces every day." It is about building good, quality patterns.
I help patients track their water intake by taking a regularly used bottle and putting three rubber bands on it. Each time they drink one bottle, they move the rubber band up to the top. This helps if they have a hard time keeping track of what they are doing.
You can think of other creative ways to help patients integrate healthy strategies to prevent lung damage. The World Health Organization also has some tips.
Social Distancing Training
Here are some things to remember about social distancing:
- Teach people how to self-advocate
- Assess how well people can communicate from 6' apart
- Role-play different situations in the community
Another educational aspect is social distancing, a whole new world for all of us. As many of our states are opening up, we must remember that our seniors are still recommended to stay at home. Many of our patients are doubly at risk because they are older and have compromising health conditions on board.
We can support social distancing with this population in many different ways. The CDC also has some guidelines:
- Stay 6 feet away from others
- Inside your home
- Avoid close contact with people who are sick.
- If possible, maintain 6 feet between the person who is sick and other household members.
- Outside your home
- Remember that some people without symptoms may be able to spread the virus.
- Stay at least 6 feet (about 2 arm lengths) from other people, especially if you are at higher risk of getting very sick
- Avoid crowds and poorly ventilated spaces
- Being in crowded places like restaurants, bars, fitness centers, or movie theaters puts you at higher risk for COVID-19.
- Avoid indoor spaces that do not offer fresh air from the outdoors as much as possible.
- If indoors, bring in fresh air by opening windows and doors, if possible.
We can model social distancing during treatment sessions as long as we are keeping a patient safe. I work with an occupational therapist who helps in the patient's kitchen. She only breaks the six-foot separation rule when she needs to keep a patient safe from falls. In our current treatments, we can do them outside if the weather is nice enough. I have a patient that does the treatments outside because I also have occupational students working with me, so I have to keep them separate from the patient.
Figure 10 is a picture of Gail with one of our patients, who is 94.

Figure 10. Gail was treating a client outside.
There are some screening opportunities to do right now as well. For example, she usually does a circuit class in our facility's gym. We cannot do that right now because the patients are not allowed to be in the gym. We have moved therapy to the parking lot (weather dependent). She does her fitness class in three separate places around the building. Patients can come out on their patio and participate as long as they are safe. They can also participate in the parking lot. We strap a speaker to a desk chair and push it around the parking lot, and she uses a megaphone.
How does that relate to therapy? I can go to those classes and then screen people by staying six feet away. We have identified people who have had worsening conditions, even things that are not related to COVID that need to be addressed. I have also found that people feel depressed because they are socially isolated and need additional support services there. As a therapist, it has been helpful to put eyes on the patients to make sure that they are doing well during this difficult time.
Strategies for Cognitive Impairments
Many therapy professionals work with older adults with dementia or other cognitive impairments. That poses a lot of challenges for COVID-19. Some things that have been done in different memory care facilities and assisted living are using verbal cues and verbal signage. If directions are in big, bold print, it makes it easier.
I talked to an RN named Kennedy Garcia, who works in a Colorado hospital. She said many of the patients who live in long-term care, memory units, or assisted living memory units are experiencing more agitation and behaviors. Part of that is about the disconnect for human connection due to PPE. They also do not see any of their loved ones. This is a time for therapy professionals to get involved because we can assess potential dementia-related behaviors that may worsen during the global pandemic. We can come in and train staff on how to reduce those behaviors and provide environmental training. This includes using music or lighting to help with those situations. You can also get creative with the activity department and create social interaction while also social distancing. For example, we work in an assisted living facility with a large kitchen. The folks that have cognitive impairments are positioned around the counters so they are not sitting right next to each other. Those are some of the contextual modifications you can do.
We also want to communicate concerns to providers. We know that many patients are not reaching out to their physicians, especially if they are struggling with telemedicine. A lot of things are going unaddressed. If you know that your patient would have had a routine doctor's appointment but did not go because of COVID, do some assessments and get that information to the providers. This prevents the situation from going unattended and promotes therapy's importance with your providers.
Figure 11 is a photo therapist with her dog that she takes out into the community.

Figure 11. A therapist with her dog.
She also has a pin that says, "Six feet away, please." It helps other people recognize the client wants to observe social distancing. I had a patient with low vision that used to wear a button that said, "I have low vision." That way, the button was helping to self-advocate.
Energy Conservation Training Post-COVID19
Fatigue and malaise are prominent factors for patients with COVID, and therapy professionals can address this in treatment plans. We see patients with mild cases of COVID getting better after about two weeks, but those with severe cases take six weeks or longer. Modulating that energy expenditure and making sure they spend the energy most effectively is an integral part of recovery.
On top of that, we also see people become deconditioned because they have been so socially isolated. They are not engaged in as many activities, not getting up as much, watching more TV, and are more sedentary. We have to address energy conservation and recovery, even with patients that do not have COVID-19. We want to advocate for therapy in situations to help people get back to their daily routines.
Community Mobility Training
Did you know that places like grocery stores are removing benches and tables? It is to reduce the risk of crowd gathering. This is detrimental to clients that need frequent breaks and who are now struggling with community mobility. It is a good idea to ask your older adult patients if they have noticed any changes that would affect them. A family member may need to assist them if so.
We already talked about doing infection prevention when in public. We can help older clients order groceries online for pickup or delivery if they choose this option. They can also access medical appointments and social connections virtually if community mobility is not an option.
Address Caregiver Burnout
We have to be considering patients' caregivers during treatment planning. This is because if a caregiver is overwhelmed, then not only is our patient at risk, the caregiver is as well. During COVID, many families have had their lives turned upside down, including personal and professional caregivers. We have families that have had to pull loved ones out of nursing homes or adult day programs to reduce the risk of COVID. It is an excellent time for therapy professionals to come in and assess the impact. Additionally, caregivers may have kids at home and not in school.
Caregiver burnout risk is at an all-time high for older adults, and therapy professionals have to consider this in their profiles for their patients. If a caregiver is showing signs of burnout, such as tearfulness, statements of feeling overwhelmed, being too quick to get irritated, your radar should start to go up. I encourage everybody to find a caregiver burnout assessment. You can do a quick run-through or even do a self-reporting questionnaire. You can say, "While I do treatment with your mom today, do you mind filling out this form for me and giving it to me at the end of treatment?" It also gives you ideas about how to help them.
I had a patient who had dementia and Parkinson's disease and was a professor before she retired. As she got sicker, she had professional caregivers coming in to take care of her. They were doing a great job, but they reported that she was not engaging in activities and was becoming agitated towards dinnertime. The caregiver would put her in her comfy chair, put her feet up, give her a blanket, and turn on a show, which sounds like something we would all like to do. Instead, she would get more agitated and started saying nasty things to the caregiver, which led to caregiver burnout. I suggested she take the caregiver to the kitchen to see if she could get her engaged. She started giving her tasks to do every day, such as putting vegetables into the salad or making a cookie tray for the table. These simple tasks helped her agitation level come down, so she was more cooperative for bed, and the caregiver had less strain.
There are different ways to look at manipulating people's routines that can support the caregiver and their overall well-being while also supporting our patients. If your caregiver shows signs of burnout, make sure that you know about resources in the community. Is that safe to bring in more non-medical care providers during COVID? You have to be able to have those conversations with people. If you have a counselor or social worker on your team, I encourage you to refer to them, and they will be able to support your plan and the caregivers' and patients' mental health.
Improve Social Connection
We can incorporate social connections into treatment plans as well. If you have a patient in the hospital or rehab, think about virtually bringing a patient's family member into the visit. Even if they are unwilling to use technology, you probably have a computer or device. Even if they wanted to show their family what they did during treatment, bring that into the treatment plan and have them engage. Socialization is critical right now for a lot of our older adults.
Focus on the therapeutic use of self. Think of ways that you can improve that social connection. I have taken pictures of flowers as an example. Be mindful that 12 million Americans over the age of 65 are alone. If you work in the home, you may be the only person they see. This is because family and neighbors are not stopping by as much. Take the time, focus on therapeutic use of self, and train patients on technology options to increase socialization.
Figure 12 is an image of the patient Claire, and these are her chickens.

Figure 12. A client and her chickens.
This was during a telehealth visit. We started talking about what she does during the day and what brings her joy. She said, "I'll be right back." She went, got her little chickens, and introduced them to me via telehealth. It is all about the therapeutic use of self, and I felt good when we both left that visit. Make sure you are putting your heart into your visits.
Expand Feelings of Purpose
Socialization and connection can expand feelings of purpose. We also need to help patients feel like they are contributing somehow. They can write a letter to somebody or support a meaningful project, which gives them a goal.
I once had a patient in a skilled nursing facility tell me that life is over when you no longer have something to look forward to. Right now, there are a lot of things they cannot do. They may not be able to go to holiday gatherings, graduation ceremonies, weddings, et cetera. What can they look forward to? What can they participate in? You can help them manage that as they do not have as much support as before. Their family members may still be coming over to visit, but they also may be overtaxed due to their own lives right now.
Promote Comprehensive Self-Care Routines
We can help patients establish positive self-care with routine exercise, getting outside, and making sure that they initiate some socialization, even if it is just a phone call. We can do that with checklists, alarms, and reminders.
Figure 13 is an image of our exercise class in the parking lot.
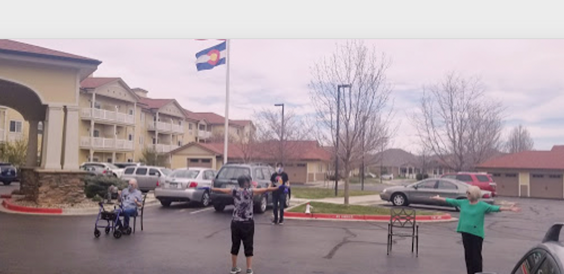
Figure 13. Exercise class outside of a skilled nursing facility.
You can see that there are three patients in the picture and there are other patients outside of the picture. This is sometimes the only thing they will engage in during the day. If that is what they are willing to do, let's do it.
Train on Assistive Technology
Training with assistive technology means learning about smartphones, tablets, and computers.
A grandparent may wish to communicate with their grandchildren but do not know how. Or, a client may need to set up a telemedicine appointment. Many older people are falling through the cracks in our healthcare system because of a lack of technology knowledge. They can easily get frustrated or overwhelmed, and we can help with that.
Some organizations are making donations of iPads and smartphones. You could give those to your patients, or you can clean them and rotate them through your facility. We have also been taking time to provide treatments with patients and making it a measurable goal. This will help the patient be independent in making and participating in doctor appointments. We have gotten good feedback from patients who said they would never have made a doctor's appointment if we had not helped them.
As an example, we had a patient whose cardiologist recommended that he download an app called Kardia to measure his heart performance and then send the results to his physician every day. We put in our treatment plan that he would be independent with that. Within two days, he could do his electrocardiography (EKG), save it to his email and then send it to his physician. Without us, I do not think he would have done that.
Telehealth
We are also allowed to do telehealth now. Authority was granted under the Coronavirus Aid Relief and Economic Security (CARES) Act, including for Medicare and other insurance providers.
We have made decades of progress in a matter of months when it comes to telehealth. Many states have already pushed for having a permanent change in this area so you need to find out what is happening in your location. You may even be able to advocate for telehealth to remain as a long-term treatment option.
It is a positive shift in many ways, including what it does outside of COVID. For instance, if you do not live in Northern Colorado, I can not see you. Now, I can treat anyone who lives in a 200 mile radius from me. I had a patient that needed a home safety assessment and lived too far away. I was able to help via telehealth, and I hopt to help more people like that.
Providing Telehealth
When you begin telehealth, you need to consider that different states function in various capacities. Know your state rules and regulations, follow your employer's recommendations, and look to your national organizations. Insurance carriers are providing telehealth in different ways. You can do a telephone visit for a Medicare patient, but in the state of Colorado, we cannot do that for Medicaid. We have to know what we can and cannot do based on insurance providers. That is a shift for us because we are used to billing similarly across third-party providers. Reimbursement is different now, depending on whoever is paying the bill. And, make sure that you know how to bill. If you need a cheat sheet, ask your provider or employer to provide that for you. I know we have one for the major providers that we constantly update because their rules and regulations are changing fast as well.
Learn Telehealth
When you are jumping into telehealth, I have some recommendations. Take some continuing ed. There is continuing ed right here on this platform, which is excellent. Make sure you dress professionally. Just because you are at home does not mean you want to be doing treatment in your pajamas. You also want to decrease clutter and distractions.
For established consent, somebody needs to agree to telehealth. You also need to document where you are and where your patient is. For example, if I provide telehealth services, I may need to be licensed in another state.
You can consider a mixture of in-person and telehealth visits. You can practice coaching your patient via telehealth as well. I have a patient that had a shoulder procedure done. She wore a cute outfit on telehealth, but I could not see her shoulder. I had to ask her to wear a camisole or tank top to see her incision. It was not ideal, but it had to be done on telehealth due to COVID precautions. When wearing a tank top, I could see how her shoulder was moving when accessing high cupboards or doing other activities.
There is a lot to learn about telehealth, and it is not as simple as any of us thought it was going to be. I encourage you to try it if you have the opportunity. In my opinion, telehealth is here to stay in some capacity.
In-Person vs. Telehealth
If you have to decide whether or not to do in-person visits or telehealth, you want to work with your management company to develop a protocol for that. Here are a few questions to consider if you are doing that:
- Is the patient COVID-19 positive or been exposed?
- Can goals be met via telehealth?
- Can the patient participate?
In the above example, my patient's daughter had COVID so I could not go into the home, and she could not go into a clinic. Luckily, my patient's shoulder had a beautiful recovery. Things to ask in these scenarios are:
- Can the patient participate?
- Do they have the equipment?
- Do they have low vision issues?
- Can they hear?
- How are they cognitively?
Some situations can be considered discrimination if you say somebody cannot participate in telehealth. You also have to base this on your organization. If an organization is required to provide reasonable and acceptable accommodations, you will want to pursue that and see what options are available.
There is a service delivery guide that comes from AOTA. It is a flow sheet that goes through different questions, and it points you to yes or no, and then what to do. If we can treat somebody via telehealth and meet their goals, let's keep them at home and reduce their exposure. If you need to see them in person, then go ahead and see your patient. However, you need to show that you have done your due diligence to analyze the situation.
Therapy's Distinct Value in Mental Health
One learning outcome is about identifying mental health issues related to COVID. We will take a comprehensive view of mental health first. The WHO defines mental health as a state of well-being in which the individual realizes their abilities to cope with the everyday stresses of life, can work productively and fruitfully, and can make a contribution to their community. Therapy services and mental health aim to help all individuals develop and maintain positive mental health, prevent mental ill health, and recover from mental health challenges to live whole and productive lives. I think we could actually take the word "COVID" and plug it in here; "develop and maintain positive mental health despite COVID-19." It is time to look at mental health as therapists.
We want to talk about mental health in general because practitioners must be familiar with how we can move through the world of mental health. Even if we do not work in a mental health-focused facility, it is easy to leave mental health aspects to the social workers, counselors, physicians, et cetera. Therapy can be a vital part of supporting someone.
AOTA has another flow sheet that allows us to see where people may fall on the continuum of mental health. We are not just looking at people that have schizophrenia or another mental health diagnosis. We have to be able to assess mental health across all populations as it is fluid. Despite having a diagnosis, people move through great times with mental health and through bad times. We have to be able to identify how mental health impacts ADLs.
We want out clients to flourish. This means they have high levels of practical well-being and positive functioning, with or without mental illness. You can have somebody with a list of mental illnesses in their history, but that does not mean that they are poorly functioning.
We then move from flourishing into positive mental health. We are happy if our patients fall into this category. It means they feel good emotionally, do well functionally, have fulfilling relationships, and cope with challenges. If we can say they are dealing with COVID-19 in a healthy way, that is great.
Signs of Becoming Mentally Unwell
We may start to see patients becoming unwell and experiencing symptoms of mental illness. This may be due to situational stressors, which is why I bring this up during COVID-19. The pandemic may be a catalyst. The CDC recognizes the fear and worry over health and our loved ones' health. If a patient has a child who is an ICU doctor or a certified nursing assistant, they may be worried.
Pay attention to changes in sleep, eating, or an increase in alcohol or drug use. They could demonstrate signs of depression, anxiety, or low levels of functioning. We may also see worsening of current mental health issues like schizophrenia or bipolar disorder.
The CDC states that mental health problems can present as physical complaints, such as headaches or cognitive issues like memory loss or difficulty concentrating. The CDC also recognizes that doctors are likely to miss mental health conditions on their assessments with patients that have underlying health conditions. Visits may be primarily focused on those other conditions, and they do not necessarily have time or space in those visits to address those factors. This is when therapy can come into play.
In a moment, we will take about some assessments available. Here are some signs and symptoms in clients that have been reported by health care professionals.
- Worry over contracting the virus
- Sadness and depression
- Loneliness
- Decreased initiation of self-care
- Disorientation to time
- Fear of dying alone
- Decreased joy
- Does not want to get out of bed
Post-intensive Care Syndrome
I also want to bring up post-intensive care syndrome (PICS). I recently did a presentation with a therapist who specializes in cognition. It is anticipated that we may see a higher frequency of PICS after severe COVID or other critical illnesses. PICS can persist after a patient returns home and involve their body, thoughts, feelings, and mind. It can also show up in family members. You may want to do a deep dive into this if you spend time with patients during their post-ICU treatment.
Additional Signs of Becoming Unwell
In addition, therapy professionals report that people are showing signs of increased struggles with sobriety and concern for their family members. Family discord occurs because families are stressed. Other results can include weight gain, sleep problems, and stress over finances. We have had a few patients that have attempted suicide. There is also fear over the lack of supplies, like PPE.
Goal and Treatment Ideas
Listening is vital when picking up clues of someone experiencing mental health decline or dysfunction. A quote from William Osler says, "The good physician treats the disease; the great physician treats the patient who has the disease." Some of the things that we might hear are that "life is too hard," "I do not know how this will ever get better," "I feel trapped in my body," "I do not think I am smart enough to do this," "Nothing I do matters anymore," "I do not feel like getting up in the morning," and "I do not think there is anything good happening to me." All of those things are red flags, and the therapy professional can start to keep track of those. If you hear them say any of these things, explore that with your patient. Do not shut it down. You want to be watching for signs and listening to them. You might see poor self-care, tearfulness, irritability, or withdrawal, which is essential to consider with COVID. There may also be significant tiredness, low energy, sex drive changes, or excessive anger. If you see that, you want to keep that on your radar as you build it into your treatment plan.
8 Areas for Addressing Mental Health
The eight areas to jump into for mental health are emotional, financial, social, spiritual, occupational, physical, intellectual, and environmental. You may want to complete multiple assessments to get a lot of great information across all eight areas. We know that mental health can be considered invisible, but we do not want to fall into that trap.
Assessments
If you are not sure how to bring it up with your patient, you can always say, "During COVID, I am trying to do more assessments with patients looking at mental health. I would like to do one of these assessments with you." You can then see if they are open to that.
There is a stigma when it comes to mental health. If you do not want to use "mental health," you can just ask a patient how they are feeling. Ask about how their mood is and what they are thinking about. I will sometimes ask people, "How are you feeling in your heart these days? You look a little stressed. Are you worried about your family?" It is an excellent time to consider the therapeutic use of self.
I want to highlight all assessments that you can use with your patients. If you are not familiar with these assessments, I have links and resources so you can investigate them and determine if they are the right fit for your patients. If you have not addressed mental health, it is a great learning opportunity right now.
Depression Anxiety Stress Scales. The first assessment is the Depression Anxiety Stress Scales. It is not an therapy-specific tool, but it is a helpful screen. This one has 42 items that people self-report on, and there is a shorter version. It looks at depression, anxiety, and stress and uses a four-point severity and frequency scale to rate that. They can answer to the extent that they have experienced each of those symptoms within the last week, which is why I like it for right now as everything is changing so quickly.
Falls Efficacy Scale. The Falls Efficacy Scale is one that I pulled in to address mental health. The fear of falling increases the potential to fall, leading to withdrawal in social engagement and a decrease in initiation of activities. Ultimately, this can lead to depression and feelings of loss and fear. If we can increase someone's confidence in fall prevention, we can likely increase their overall satisfaction in their daily activities. The Falls Efficacy Scale indicates the level of perceived confidence an individual has about carrying out everyday activities without falling. The scale was one of the first to assess older adults' perceptions. I always like to know what my patients think about themselves and their performance levels. It solicits the older adult's perception about a fall risk, and it does not measure their objective performance in any way. If you are worried about the physical or biomechanical aspects, you will want to bring in another assessment.
The scale also focuses on confidence. It does not measure balance, speed, or others that we usually think about with falls. It has assessment items that are more functional and oriented. Therapy professionals love the word "function." We know that this can lead to reduced participation in ADLs because it can lead to falls. We want to stop those falls from happening and help people get more confident going back to their ADLs.
PHQ9-Patient Depression Questionnaire. The next one is the PHQ9-Patient Depression Questionnaire. It is one of the most validated tools in mental health, and it is not just designed for therapists. As such, physicians are very familiar with this. It is fast to deliver. As lifestyle changes are happening, I suggest that even if you see patients you have known for a while, this is a good one to bring into the conversation.
Occupational Circumstances Assessment Interview Rating Scale. The last assessment is the Occupational Circumstances Assessment Interview Rating Scale. This is a semi-structured interview and rating scale based on the Model of Human Occupation. It helps us understand the extent and nature of a client's occupational adaptation. We all have to do a lot of that right now, including data on clients' goals and readiness for change. I like this assessment because of the customization factor. If you have a certain relationship with a patient and want to talk about things casually, you can modify the questions.
The questions are fill-in-the-blank. For example, a query may be, "How has your routine changed over the last three months since ____?" The blank could be since COVID-19, shoulder surgery, and so on. Another critical question is, "Are you satisfied with your daily routine?" It lets us bring COVID-19 impacts into the questions. This way, we can get a personal profile based on that patient and learn how COVID-19 impacts their routines and mental health.
Assessing Suicide Risk
All of us need to be able to assess suicide risk. You may notice certain behaviors, such as talking about suicide, hoarding medications, expressing purposelessness, substance abuse, practicing social withdrawal, or mood changes. These behaviors may indicate that a suicide risk is going up. Another factor to consider is if they have access to firearms. If they are in the hospital and are going home, ask them if they have a gun.
Do they have a history of suicide attempts? Somebody who has attempted suicide in the past is more likely to try to commit suicide again. Have they had a triggering event? Have they recently been in the ICU? Have they experienced surgery or a heart attack? These are some questions that you can ask when assessing suicide risk. How are they coping? Are they thinking about dying? Are they thinking about hurting themselves? Have they thought about how or when they would do it? These are vital questions to ask if somebody is showing a risk. If you find that a patient has established a plan, that is when your radar needs to go up, and you need to take action to follow that information.
I had to ask these questions the other day when I did a PHQ9 with one of our patients. There were some comments that I was concerned about, but when I started diving into it, I found that she has a profound faith. She said, "I would never do that, and I have no plans to do that. I just know that I am at the end of my life, and I am ready to die." That is different from being actively suicidal. We have to make sure that we are getting the correct information and doing what we can to keep our patients safe.
Always keep the National Suicide Prevention Lifeline with you and know when to refer someone. If you ever come into somebody's situation, whether it is a hospital room, their home, or assisted living, and if they have attempted suicide, you do not leave the person alone. Call 911 or an emergency number. Try to find out if they are under the influence of alcohol or drugs. You also want to get their friends or family members involved. This is a dark topic, but we know that suicide risks are increasing.
I like this quote from General David Satcher, saying, "There is no health without mental health." You can work on everything under the sun, but if you have a patient struggling with mental health, likely, a lot of your treatment interventions will not be productive. You want to bring mental health first and foremost."
Review
We have talked about integrating relevant, educational information into treatment plans regarding COVID-19, implementing effective infection prevention strategies into your evaluations, comprehensively identifying and addressing occupations directly and indirectly impacted by COVID-19, and identifying mental health issues related to COVID-19. We are responsible for these things anyway, but we have to look at them differently because of this pandemic.
Conclusion
In closing, I would like to leave you with this quote from occupational therapist Kate Hackett: "As occupational therapists, we care about our client's mental health, their social work, education, and family life as well as their particular medical condition and symptoms. We don't see any of these factors in isolation." I love that word tying together with isolation since we have so many older adults that are isolated right now. This is a great quote to hang up in your rehab gyms and hospitals. Put it on your clipboard when you are doing home care.
I hope this triggered some ideas for you with treatment planning and inspired you to continue to provide support for older adults at high risk with COVID.
References
Available in the handouts.
Questions and Answers
Which apps do you recommend for breathing?
I previously mentioned the Breath Ball. There are several apps online for breathing. I cannot promote one over the other because I like different apps for different reasons for patients. Breath Ball is one that I have used in the past.
Do you know how NIF is getting their PPE? Are they giving it to families to keep them safe?
I think it depends on where you are. Colorado had a hard time with that in March, and it has since gotten better. You can try to go to Central Supply and ask what they can do or how they should provide things to patients. I have had some patients' families somehow acquire face shields. I have had a patient that had a daughter in a facility. She had previously been on a ventilator and was at high risk. That family obtained several face shields and had them available for all the providers seeing her. We have worked with some non-medical home care agencies with PPE and who have given us some. I do not have a lot of information on that.
What do you do when you go into homes? Do you remove your shoes when you go inside?
I do not remove my shoes to go into the homes, but I have foot booties. That depends on the house, and I will wear them if it is a concern. If we remove our shoes, we are walking around barefoot. Unless the local recommendations are different, the CDC is not saying to remove your shoes.
Are people providing telehealth for SNF settings? You showed some options that you were doing. What are you seeing?
People are providing telehealth at SNFs. Again, I am not an expert in that. With being able to do telehealth in specific hospital settings and SNFs, the allowances came out later. However, if you go to the CMS website and look up skilled nursing facilities and telehealth, some resources should be there.
What about if someone was asking about mental health resources? You did give some resources from AOTA and a great reference list. Are there any other places to go for that?
I like the American Psychiatric Association for resources. I also want to look into whatever social workers are using. That may just be because I have a degree in social work, so I like to tap into that. There are a lot of ways that social work and therapy blend. There are some great apps as well. If you search for apps related to mental health, depression, or assessments, there are some quality resources that you can get on your tablet or phone.
Citation
Covell-Pierson, K. (2022). Covid-19 with older adults: An update. OccupationalTherapy.com, Article 5486. Available at www.occupationaltherapy.com

