Editor’s note: This text-based course is a transcript of the webinar, Healthcare Professionals & Covid-19: How to Navigate a New World with Older Adults, presented by Krista Covell-Pierson, OTR/L, BCB-PMD.
Learning Outcomes
- After this course, participants will be able to describe COVID-19 information and resources to be able to implement this into treatment plans with patients and families.
- After this course, participants will be able to list effective infection management strategies.
- After this course, participants will be able to identify mental health issues related to COVID-19.
Introduction
Speech-language pathologists have a role in older adults’ lives amidst COVID-19 because we address activities of daily living (ADLs), safety, quality of life, mental health, and other areas that are directly impacted. It has been a scramble for all of us to learn what to do during this time. We have had to move through this situation uniquely depending on our work setting and what is going on for us personally.
When COVID-19 hit, I often found myself in tears because the people I had been caring for were at high risk for the virus. I thought about the patients who live in skilled nursing facilities that were no longer allowed to have visitors. Some of my colleagues were diagnosed with COVID as well. We all have stories that we could share around the global pandemic and how it has affected the people we care about. Figure 1 is an image of me with a patient pre-COVID:

Figure 1. Krista with a client before Covid-19.
Figure 2 is an image of me a couple of weeks ago:

Figure 2. Krista after Covid-19.
We all miss the things we were able to do in the past such as smiling at our patients without a mask. It has been a process to feel like we can provide quality care. No one is an expert in COVID-19, but we are going to do the best we can with the information.
Our World Now
Earlier in the year, we started learning about this virus that many people did not take seriously, including me. We heard stories from China and Italy but when things started to get closer to home, it felt more alarming. All of a sudden, a wave of change happened for all of us. The impact of this virus has been felt by people across the globe. Millions of people have lost their jobs, and health care has been scrambling for personal protective equipment (PPE). We have watched the number of people in hospitals go through the roof. We all learned what it meant to be an essential worker. We started to hunker down in our homes in ways we never have before. The US government has been sending out stimulus packages at an unprecedented rate. We each have a story about how we have managed the situation.
Our older adult population has been significantly impacted by COVID-19. According to the Centers for Disease Control and Prevention (CDC), more people have died from COVID who are over the age of 65 than any other age. It makes everything harder when someone is hospitalized and they cannot have visitors. I have a family member in the hospital right now and he cannot have visitors. He is 89 years old and has dementia. Nursing homes are a breeding ground for the virus, so those residents have been greatly impacted. Older adults are more impacted because they are alone in their homes for days on end. They do not necessarily have the same capabilities that we do with technology. That is a great place for speech-language pathology to step in. As we continue to move through the pandemic, we are going to bring the focus on our profession in hopes of providing support, education, and ideas about how we can do our jobs safely and effectively amidst this turbulent time.
Where Do We Fit with COVID-19?
While many of us live in places that are in the process of reopening, the message to older adults and those with compromised immunity continues to be that staying at home is better. Older adults in our community are still experiencing occupational disruption. They are showing to have more falls, overall diminished quality of ADL, decreased life satisfaction, and declining mental health and cognition. We are seeing an overall breakdown in people's ability to function at their best for multiple reasons right now. This is where healthcare professionals can shine. We may not be experts in COVID-19, but we are experts in helping people that are struggling with their communication. No matter what setting we work in with older adults, we can help and have an impact.
Things have changed quickly over the last several months and have impacted our profession. We have to discern what is appropriate for our unique circumstances and clientele. We must continue using clinical judgment, empathy, and safety. We may need to make decisions quickly and pivot directions depending on what is happening with COVID-19. Not everything I talk to you about today is going to apply to every single person. Wherever you are, I am hoping that you can adapt what we talked about according to your setting.
Older adults can mean anyone from 65-year-old to a healthy, vibrant 90-year-old. I was hiking last week and met an 84-year-old and an 80-year-old. When they told us how old they were, I was shocked because I do not typically see older adults at that high level of performance. We can talk about the well elderly, and then we can talk about a 65-year-old who has Parkinson's and other comorbidities. As we look at this range of people and the settings that we work in, we have to be creative. I have a patient who is 72. She has cancer but works part-time as a paralegal. Now that her law office is opening up, I am helping her with going back to work and reducing her potential exposure. She is considered high risk but wants to go back to work.
The recovery process from COVID for a lot of our patients is going to be quite long. We have had patients that have been in the hospital for over 30 days. Some have come home, but others have been put in long-term care after being in skilled nursing.
We want to integrate COVID-19 information resources. We then implement these into treatment plans with patients and families. There is a ton of information about COVID-19, and it is important that we address COVID as part of our patient's profiles. In order to do that, we must have the appropriate information ourselves and know where to go for that information.
History of Coronavirus
Learning about COVID’s background helps us give quality information to our patients and their families. It also helps us make decisions, as well as reduce hysteria and anxiety for yourself, your patients, and their families.
According to the Centers for Disease Control, human Coronaviruses were first discovered in domestic poultry in the 1930s. It was first seen in humans in the 1960s. The word Corona means a crown, which refers to the crown-like spikes on its surface.
Types of Coronaviruses
There are seven types of Coronaviruses that can infect people. Four of them are most likely what causes the common cold. The other three types cause severe lung infections, which is what we are seeing presently:
- MERS
- SARS
- COVID
Some of you may have heard of Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). It is believed that MERS, SARS, and our current virus have originally only been in animals. We now know that they can transfer to people.
The initial discovery of COVID was in Wuhan, China. When patients became infected, they had a link to a seafood and animal market. That introduced our first understanding that this was an animal-to-person spreadability. As more people became infected who did not have contact with that market, it became obvious that the virus was now spreading person-to-person. In the middle of May, it was present in 212 countries and all 50 of the United States. That spread is something that we have never seen before, and there is no natural immunity to it. It can cause mild to severe illness, and the most severe illnesses will most likely show up for people who are over the age of 65 or those who have underlying health problems.
The name of our current virus is SARS-CoV-2 and it causes COVID-19. Another example of a virus causing disease is HIV, which causes AIDS. The 19 refers to the year that it was discovered, which was 2019.
Go to Trusted Sources
There is a lot of information circulating about COVID, so it is hard for people to know what to believe or where it comes from. If patients and your families have questions about COVID, we have to provide them with good sources:
- The World Health Organization
- Centers for Disease Control and Prevention
- Federal Drug Administration
- National Institutes of Health
- Department of Health and Human Services
- State health departments
- City and county health departments
We should not be sharing news that we get from Facebook. We have to use reliable organizations that we can share with our patients. Even though politics are being brought into the Coronavirus conversation, we do not want to be talking about that with our patients.
We want to refer people to sources like the World Health Organization, which has a subgroup of the United States. The CDC has information that is easy to read and has graphics. It is part of the Department of Health and Human Services, which is cited here as well. Its purpose is to protect Americans from health threats both here and abroad.
It is important to have your client and their family know where to go for information because they may go through a healthcare system, hospital, rehabilitation center, home health, and so on. There is a possibility that after going through those programs, they may get diagnosed with COVID. In those cases, we want them to know where they can go for updated information.
It is important for them to look at their own state health departments as well. I live in Northern Colorado, which is close to a hotspot in Greeley, Colorado. I needed to know what was going on there, as well as in my own county. You want to educate your patients about that and take the time to help them get access to those sources.
COVID-19 Versus the Flu
Some of our patients still think that COVID and the flu are similar. As a healthcare professional, you have the language and knowledge to talk about the commonalities and the differences. Some of our clients are overwhelmed with new information, so we want to clear up any confusion:
- Commonalities
- Cannot be treated by antibiotics
- Droplet transmission
- Handwashing helps with prevention
- Both respiratory
- Differences
- Spreadability
- Vaccine only available for the flu
- Antiviral medication can treat the flu, but no medication available for COVID
The flu and COVID are both caused by viruses that cannot be treated by antibiotics. The flu is caused by the Influenza virus, which is similar to how COVID-19 is caused by the SARS-CoV-2 virus. Sneezing and coughing release droplets into the air and gets into other people's eyes, nose, and mouth. It can also be transmitted if someone touches their eyes after they have touched an infected surface. Handwashing helps with prevention.
Spreadability is one of the biggest differences. With the flu, we know that people can experience symptoms for one to four days after being infected. It can be spread in the first one or two days before a person realizes they are sick. With COVID, people are typically experiencing symptoms for two to 14 days after being infected. They are contagious the entire time. Not everyone experiences symptoms. They may move through the world sick and spread it around without realizing it. There is a vaccine available for the flu, but not for COVID at this time. Antiviral medication, like Tamiflu, can be used to treat the flu. We do not have anything available for COVID yet.
Goal and Treatment Ideas
I want you to have ideas that you can put right into your care plans. Remember your responsibilities. Depending on your setting, you should be screening people for COVID signs and symptoms every day. We should be doing temperature checks for ourselves as well. At my company, we request that patients get screened by the therapist, as well as have the therapist screening themselves twice a day. We use a non-contact thermometer that you use by pointing it to your forehead. If somebody spikes a fever, that is our first red flag. If somebody has a dry cough and feels tightness in their chest, we call the healthcare provider.
We are also providing mobile screenings. We can conduct these in people's homes. This is different if you are in a hospital or skilled nursing setting. We are also screening patients every day and asking the people in their homes about where they have traveled. We then take temperatures and ask about possible signs and symptoms of COVID. If somebody has spiked a fever or is showing symptoms, we do not complete the treatment. Instead, we get in touch with the home or care provider. Your work setting should be showing you how to screen your patients for COVID. As we move forward, we need to make sure that we are remaining diligent.
We had a speech therapist who also works in the hospital. She went to work and felt fine, but when she was screened at the hospital, she had a slight fever. The biggest concern is if the fever is approximately 100.4 or higher, and hers was just under that. Her employer sent her home, and by that evening she was in the hospital on a ventilator with COVID. She had been in front of other patients for two weeks prior to that, so everybody had to be contacted. Nobody else was sick that we could connect to her experience and she is now better. I share that story because it drives home how important this is. We have to keep people safe and do those screenings.
Empower Clients and Families
You want to consider asking your clients about their knowledge of COVID-19 right away, then share information if they are incorrect or have gathered something that is no longer true. You may also want to assess where they are getting their information. You can encourage a client to independently locate resources and add that as a goal to your treatment plan. Knowing the landscape is changing, we want to make sure that they know what to do if there are changes in our communities or they are no longer tethered to us. An important part of discharge planning and following their goals is to make sure that the information is sticking and that they understand where to get it. I also recommend having a handout. It could be from you or your agency about infection control, resources, websites, and local organizations that provide information. This way they can have it at their fingertips.
Use of Personal Protective Equipment
It is important to talk about effective infection prevention strategies if you are working with patients who have COVID or are presumably positive. If they are not getting tested, adherence to your organization's infection control policies is critical. I cannot emphasize enough how important it is for all of us to protect ourselves, our families, and our patients.
Here are some points to remember about PPE:
- Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must:
- Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE.
- Demonstrate competency in performing appropriate infection control practices and procedures.
- Remember:
- PPE must be donned correctly before entering the patient arena (e.g., isolation room, unit if cohorting).
- PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/ face mask during patient care.
- PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be developed and used during training and patient care.
PPE handout from CDC: https://www.cdc.gov/coronavirus/2019-ncov/downloads/A_FS_HCP_COVID19_PPE_11x17.pdf
You should all receive training on infection prevention recommendations by your employer. It is important to know how to put PPE on and take it off. If you do it incorrectly, you can spread the virus. If you feel like you are not getting enough training, I encourage you to look at some resources and take them to your management team. We want to make sure that everyone is getting the support they need. For example, one of our hospitals created a team of registered nurses (RNs) to help with an intensive care unit (ICU) teams. They were noticing that the way people were storing their PPE and taking it off was causing cross-contamination. Speak up if you notice something. There should be an infection control person that you can talk to as well. The CDC requires people working with folks who have COVID to have a face mask, goggles, N95, higher mask, a pair of clean non-surgical gloves, and an isolation gown.
Regarding healthcare facilities and PPE, the recommendations are being updated regularly. There are contributing factors, and depending on what they need and your work setting, it is going to be different. In the beginning, the staff at skilled nursing facilities and hospitals were pivoting by the hour to get updates on what PPE was required. I have the information that is current about the use of PPE, as well as some listings that you can refer to for your own reference.
Donning PPE
More than one donning method may be acceptable. Training and practice using your healthcare facility’s procedure are critical. Below is one example of donning:
- Identify and gather the proper PPE to don. Ensure that the choice of gown size is correct (based on training).
- Perform hand hygiene using hand sanitizer.
- Put on an isolation gown. Tie all of the ties on the gown. Assistance may be needed by another HCP.
- Put on NIOSH-approved N95 filtering facepiece respirator or higher (use a facemask if a respirator is not available). If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented. Do not pinch the nosepiece with one hand. Respirator/face mask should be extended under the chin. Both your mouth and nose should be protected. Do not wear a respirator/face mask under your chin or store in a scrubs pocket between patients.*
- Respirator: Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time you put on the respirator.
- Facemask: Mask ties should be secured on the crown of the head (top tie) and base of the neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
- Put on a face shield or goggles. Face shields provide full-face coverage. Goggles also provide excellent protection for eyes but fogging is common.
- Perform hand hygiene before putting on gloves. Gloves should cover the cuff (wrist) of the gown.
- HCP may now enter the patient room.
Doffing PPE
More than one doffing method may be acceptable. Training and practice using your healthcare facility’s procedure are critical. Below is one example of doffing:
- Remove the gloves. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so in a gentle manner, avoiding a forceful movement. Reach up to the shoulders and carefully pull the gown down and away from the body. Rolling the gown down is an acceptable approach. Dispose of in a trash receptacle.
- HCP may now exit the patient room.
- Perform hand hygiene.
- Remove face shield or goggles. Carefully remove face shield or goggles by grabbing the strap and pulling upwards and away from the head. Do not touch the front of the face shield or goggles.
- Remove and discard respirator (or facemask if used instead of respirator). Do not touch the front of the respirator or facemask.
- Respirator: Remove the bottom strap by touching only the strap and bring it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Facemask: Carefully untie (or unhook from the ears) and pull away from face without touching the front.
- Perform hand hygiene after removing the respirator/facemask and before putting it on again if your workplace is practicing reuse.
Figure 3 shows the difference between an N95 respirator mask and a surgical mask.
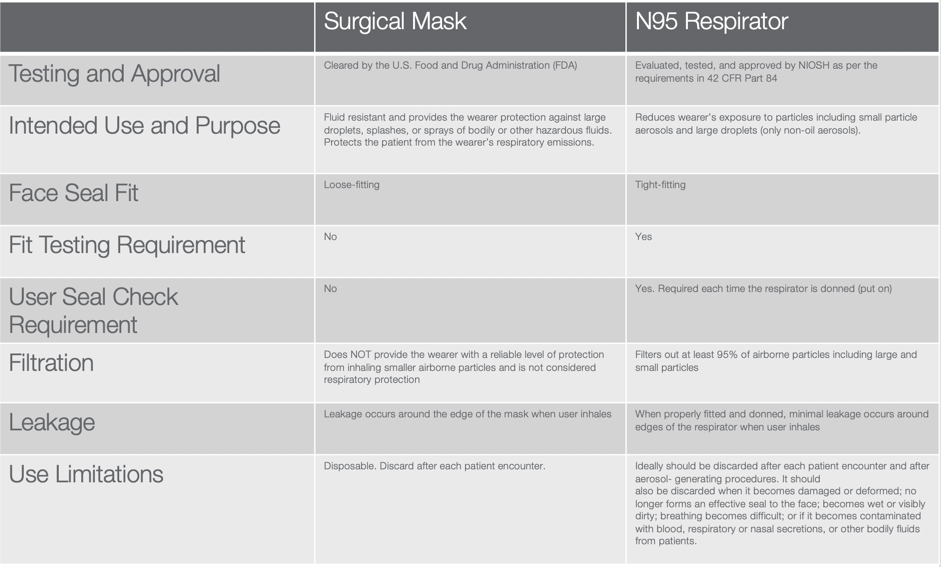
Figure 3. N95 respirator mask vs. surgical mask.
(Link to pdf of Figure 3: https://www.cdc.gov/niosh/npptl/pdfs/UnderstandDifferenceInfographic-508.pdf)
Depending on your work setting, this level of PPE may not feel that different. However, this is not the case for many healthcare professionals. We want to make sure that you all have good resources and know where to go. It is important to educate yourself in order to feel confident.
Know Your PPE Requirements
Whether or not you are seeing clients with COVID, we need to be educated about putting infection prevention practices in place every day. We have to do our due diligence and follow our local community guidelines when we are away from work as well. For example, I decided to go to the park with my kids and have a picnic. The park is open for 10 people or less and has a playground. Even though there was only one other family, I did not allow my kids to use the playground. I do not want to be the vector that gives infection to my older adult patients who are at risk. We can look to our supervisors and our local and national organizations for guidance.
Figure 4 is an image of my colleague.

Figure 4. An Image of a staff member with PPE.
If you are wearing full PPE like Jessica, it can be exhausting and tiring. Additionally, I think we should all be wearing her shirt because we should not be shaking hands, especially at work.
Safety Starts with You
For some, it may only be required to wear a surgical mask seen in Figure 5.
Figure 5. Staff taking safety measures.
The woman on the right is not wearing gloves, but you get the idea. These are two talented OTs that I have worked with for the last couple of years. They work with a company called Thrive Therapy. They have been seeing patients throughout the global pandemic in an independent assisted and memory care facility. They have been staying safe and nobody in their facility has gotten sick.
Handwashing
As healthcare professionals, we understand the importance of handwashing. It is recommended that people wash their hands for 20 seconds or more to be effective, and using alcohol-based hand rubs is fine. They have to be 65 percent alcohol-based solution or higher. We have had breweries and distilleries in Colorado that have been able to tap into those companies and get hand sanitizer and surface cleaner for our therapists.
We are required to observe infection prevention directives with our patients. We have always encouraged patients to wash their hands and use hand sanitizer. However, now they are also being asked to wear a mask. We now do supervised handwashing, which we have never done before COVID. Whatever your patients have to do will depend on the settings, but if patients are refusing to participate in infection prevention strategies, it may result in treatment being discontinued. I talked to a physical therapist who had a patient come in for treatment. The patient was refusing to wear a mask. The therapist said, “If you will not wear a mask, then there will be no physical therapy." The patient still refused.
How Speech-Language Pathology Can Help with PPE with Older Adults
I am now going to talk about developing creative ways to connect with older adult patients despite wearing PPE and practicing social distancing.
Goals for Handwashing
Figure 6 is an image of one of my patients.

Figure 6. Incorporating handwashing into treatment.
It is beneficial to set a specific goal related to handwashing. You can include factors like independent initiation if you have to remind your patient every time. Are they washing them after they do certain tasks or after they see somebody? You also want to consider how they wash their hands. Do they use soap and water or hand sanitizer, or both? You then want to talk about how to manage in public places. If they touch something and they are wearing gloves, should they use hand sanitizer on those or not? All of those factors can be built into a treatment plan for education and safety.
A goal I recommended for a patient is completing handwashing independently with proper technique, soap and water, and for 20 seconds or more for three out of three consecutive sessions. The ability to change this patient’s handwashing was a challenge, but she was in the early stages of dementia. She was able to integrate some new habits. We also put up a few signs next to her sink in order to help her remember what she was supposed to do.
You could also set a goal in regards to self-advocacy for those who are living at home. I had a home care client with a lot of family in and out of their house. The goal was that the patient will independently request all family members coming into the home to wash their hands when they arrive for seven consecutive days. This patient was passive in nature and would not ask people to wash their hands when they came in.
Talk with Patients about PPE
Make sure you are talking about your PPE with your patient and explain that you wear it for their safety. Emphasize that you work with people who are sick, compromised, or old. You can also ask the person to wear a mask to protect patients. For the greater good of others, I can get people to buy into some ideas that they are not open to.
I can give you the verbiage that I have used. You can say, “Before we start our session today, I want to talk with you about how I do infection prevention. I know you are eager to tell me how you have been doing since our last session, but let's make sure we do our supervised handwashing.” I then wash my hands in front of them and vice versa. You can also say, “I know you are going out in the community more. Tell me how you are managing your mask when you are out and about. Can you show me how you are putting it on and off?”
How often should you be washing your mask? I do not know if people are washing their cloth masks. You can include a goal about using cloth masks 100 percent of the time in the community over the next two weeks. Not everyone has been wearing a mask. We may need to have multiple conversations about that to make sure they are staying safe and reminding them of the importance for the community and themselves.
Hang Up a Picture
We have been displaying pictures of ourselves taken before COVID. You can put up pictures of your team without masks on. These photos can be individual or of your whole team. It is nice for them to see a real face. Figure 7 is an image of a nurse practitioner who I work with.

Figure 7. Krista with a coworker.
She does house calls and sees our patients at some of our facilities. It is nice for me to say, “I am going to ask that Rita comes in and sees you. Here is a picture of Rita because she will be wearing a mask.” You could also put a picture of yourself on your name tag. This can help build human connection despite the PPE in the way.
Get Creative with PPE
Here are some ways you can modify PPE creatively:
- Use masks with “windows”
- Reduce background noises
- Modify and adapt patient masks
Figure 8 is an image of the speech therapist who tested positive for COVID-19.

Figure 8. Mask with a clear window.
This picture was taken after her experience with COVID. After her recovery, she uses these masks. They are great for speech therapists and occupational therapists because they allow the ability to read lips.
When a patient has a low-voice projection, it is a reminder of how tough masks are. Due to this, we want to make sure we are reducing background noises. You can also have someone with a hearing impairment stand with their back against the wall. This helps with overall hearing, regardless of a mask.
Modifying Masks Video
There are many different things we have to consider when it comes to masks. Putting masks on and off for our older adults is more challenging than expected. This is especially the case for those who have shoulder problems, neck problems, glasses, or hearing aids. This is a video of Gail, who works with me as a personal trainer. She works in one of our independent living facilities. She figured this out for her patients in the following video.
VIDEO
Gail has since discovered an origami mask which is great because they have more space inside. It eliminates pushing down on the nose. It is great for those who have oxygen because there is nothing touching your face. We can exchange buttons for Velcro and shoelaces for elastic.
We also teach people how to don/doff different types of clothing. Wearing a mask is now part of that. You want to make sure that they are donning and doffing it appropriately. In a rehabilitation setting, we have to think about the next phase for clientele outside of the facility. It could be in their home, the community, a return to work, or assisted living.
I had a patient who had started to go back into the community and do his own grocery shopping. He had gloves, a mask, and hand sanitizer. However, he was taking the mask off from the front and putting it into the console with his gloves on. This means he was using dirty gloves, putting the mask down, taking the gloves off, and putting the dirty gloves in the console. He then touches the ignition, the steering wheel, and his face. We then needed to discuss how to remove the mask from the straps and when to wash his hands. We have to teach people how to do these things as we learn to do them ourselves. We need to have a good treatment session, as well as a simulation, even if you are in a rehabilitation setting. This is the best way to do it, rather than go out in the community and try.
There are many different ways to put infection prevention into our treatment programs. This will benefit the public, our patients, and their families. We want to empower them because this is the new normal, and it will probably stay this way for a while.
Activity Analysis
This is a good example of activity analysis and incorporating infection prevention into activities of daily living (ADLs). If you can go out in the community with your clients, you will learn a lot. Figure 9 shows an example.

Figure 9. This shows an example of an IADL where you could work on infection control.
Goal and Treatment Ideas
I am going to walk through a variety of areas that need to be looked at through a new lens for patients during the pandemic. It is time to level our treatments because we should not be addressing therapy in the same way we did prior to COVID. We need to bring COVID impact into evaluations. Your evaluation forms will most likely not ask how COVID has impacted your patients. It is up to practitioners to bring that into documentation, mindset, and plans. It has to be defensible because it is how we help patients stay functional and safe.
Since we are all working in various settings, not all treatment ideas will apply exactly as I explain them. You are not in a setting that allows for multiple treatment sessions. You do not have time to spend on that if you are in a short-term hospital situation. You can create a handout for your patients and their families to read on their own time. This can include general information, not just COVID precautions. Your team can also make an informational video that patients on your unit will watch at some point during your program. You could bring the information to a virtual platform. This way they can reduce the time that may be spending in your treatment session on that.
For those of you working in skilled nursing, I always love working with our restorative nursing program. Now is a great time to revamp your programs because they do not always have to be about exercise. Think about increasing socialization or adding FaceTime to some of the programming. This is an opportunity for creativity. As healthcare professionals, we can become leaders and tie performance with COVID's primary and secondary impacts. The client’s context is being impacted no matter where we are, so we have to consider that throughout our treatment sessions.
Positioning
Those of you who have worked with patients that have pneumonia or chronic obstructive pulmonary disease (COPD) know that positioning impacts respiratory function. This applies to patients with COVID as well. Putting patients in a prone position on their stomach improves respiratory function since there is no tissue on the backside of our lungs. When our patients are laying on their backs, that creates more pressure through the lungs and makes breathing more difficult. Moving patients into this position reduces pressure and improves the movement of air in our lungs. Being prone opens up the diaphragm, which is the main muscle used in breathing. Position change can improve recovery time and reduce the severity of COVID symptoms.
Moving patients into this position is not a new tactic. Before ventilators, putting people in a prone position was done as one of the main interventions for about 20 years. If somebody is in respiratory distress and is in the ICU, it is recommended that they remain prone for 16 hours a day. That is a long time and some people cannot tolerate that. Our hospitals are integrating programs where people are prone for four hours at a time twice a day. We also need to think about when positioning makes sense. If somebody is in the ICU, it may not be as appropriate. You can use prone positioning in other settings, such as home care or skilled nursing.
You can also help patients be functional in various positions. If they are laying on their stomach the whole time, can they watch television or listen to books on tape? This can help them enjoy that stretch of time and make it go faster.
A lot of older adults who get sick do not necessarily have to go to the hospital and be on a ventilator. If we can help them in a prone position during their recovery, that would be a great intervention to consider. You can do this with COVID patients in ICU, rehab, long-term care, and home care.
I have an example from a skilled nursing facility in Greeley, which was a hot spot that had over 30 percent of their population infected with COVID. Once the occupational therapists and physical therapists started integrating positioning with their COVID patients, they saw that they were not getting as sick or staying sick for that long.
The recommendation is to start prone positioning as early as possible. You can educate your patients on prone positioning interventions. This way if they know somebody who gets sick, they can possibly integrate that themselves.
Activity Engagement Post-Intubation
What happens if we are seeing patients after COVID? This is probably where most of us are seeing our patients. Research is telling us that helping patients get moving as soon as they are medically cleared can enhance long-term, successful recovery. The recommendation is that a patient is up for about seven days a week. This will be difficult because if patients do not feel good, it is hard to motivate them. However, we can integrate that into their treatment plan and create goals around that. We can monitor their participation, initiation, execution, and how many times they have to take a rest. We can help with that because we are good at helping people engage in meaningful activity. We may have somebody make Rice Krispie treats for their granddaughter and have someone else cut up T-shirts to help out those who are making masks. We can integrate that with sitting up longer, being on their feet, and getting supplies together. We can be meaningful and functional while also getting people moving. We also have to educate people on the importance of getting up in order to reduce the long-term struggle with COVID-19.
Promoting Respiratory Health
We need to promote respiratory health into our older adult patients’ treatment plans. Research is mixed on whether or not increasing lung strength actually helps patients prevent symptoms of COVID-19. I have information from John Hopkins University and it reads as follows:
In pneumonia, the lungs become filled with fluid and inflamed, leading to breathing difficulties. For some people breathing problems can become severe enough to require treatment at the hospital. At the hospital with oxygen or even a ventilator, pneumonia with COVID-19 tends to take hold in both lungs. Air sacs in the lungs fill with fluid limiting their ability to take in oxygen and causing shortness of breath, cough, and other symptoms. While most people recover from pneumonia without any lasting lung damage, pneumonia associated with COVID-19 may be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.
This means that whether we are working on promoting respiratory health prior to COVID, in case somebody gets it, we also need to step up our game afterward. Some things that we can do are practice diaphragmatic breathing and pursed-lip breathing. If you are not sure how to do that or you need practice, there are resources online that can help with that.
I can speak for myself and the patients I see, but I have used breathing strategies in several of my treatment plans over the years for a variety of situations, such as mental health, stress management, community mobility, and increasing activity tolerance. You could write a goal for a patient that has them complete lung exercises using the Breath Ball app for five to seven days with good technique. It is about integrating a good self-care program that somebody can stick to.
Author Tim Winton has a quote that you can understand if you have ever worked with anyone struggling with respiratory health. He says, "It's funny, but you never really think much about breathing until it's all you ever think about." I can tell you, from working with people that have had COVID, it is all you think about when you cannot catch your breath. It is a scary and insidious situation. And it's a little insidious. We see the anxiety and the breathing difficulty with our patients that have COPD as well, and we are often unsure of what came first. We want to prevent people from getting that fear of not being able to catch a breath. If we can educate people on good lung function, how the lungs move, and how the diaphragm interacts, that can allow them to stay in control.
However, I do not want to get that confused with respiratory distress. That is a medical emergency that they can breathe their way through. If they know they are getting worked up, they can keep themselves calm by doing diaphragmatic breathing. Those conversations are important to have with patients.
Promote Good Diet and Hydration
On top of the physical exercises that we can do to support patients’ lung health, we can also integrate diet and hydration into our treatments. If someone is always eating junk food or drinking diet soda, they are not going to have good effects on their overall capacity to prevent infection or get rid of an infection. We want to build up people's resiliency and immunity as much as we can.
Proper hydration is important with lung health as well because it maintains proper blood volume and healthy mucous membranes in the respiratory system. That can help us all resist infection and tissue damage if we were to get COVID-19. If our older adult patients have incontinence, they are not drinking enough water. If this is the case and you try telling them how much more water they should be drinking, they are not going to do it because it is too overwhelming. You want to start slowly with your treatment plan. If they are only drinking eight ounces of water a day, increase that to 16 ounces. You can say, “By the next time you come back, you should reach for 16 ounces every day.” It is about building good, quality patterns.
One way that I help patients track their water intake is by taking a regular water bottle that they are using on a regular basis and putting on three rubber bands, for example, if I want them to drink three of them. This helps if they have a hard time keeping track of what they are doing. As they finish a bottle, they can slide the rubber bands to the top, knowing that once they have all three at the top of the bottle, they have met their goal. Think of creative ways that you can help patients integrate healthy strategies that prevent lung damage if they were to get COVID-19.
Social Distancing Training
Here are some things to remember about social distancing:
- Teach people how to self-advocate
- Assess how well people can communicate from 6’ apart
- Role-play different situations in the community
Another educational aspect is social distancing, which is a whole new world for all of us. As many of our states are opening up, we have to remember that our seniors are still recommended to stay at home. A lot of our patients are doubly at risk because they are older and also have compromising health conditions on board.
We can support social distancing with this population in many different ways. A big way is through self-advocacy, whether it is with the patient themselves or with their family. We can design goals and treatment sessions around this subject because patients will have to adhere to recommendations. This applies if they live in a facility or if they have family visiting like I mentioned the home care patient that the family flies in and out of his house all the time, or whether they're in the community and with perfect strangers. It can feel uncomfortable to back up from someone because it feels socially strange. It is also hard for us to maybe speak up to our daughter, for example, that is so loving but is touching us all the time. We can do some role-playing with our patients in order to help them get comfortable and gain competence.
Another thing that is also important is language. Give people statements that they can say and make their own so it feels normal for them. If we just tell patients to ask people to back up, the patients are not going to do that. We want to make it as real as possible. If you are in a creative environment, you can go out with them in the community. You will be surprised at all there is to work on as a professional when it comes to social distancing.
We can also help with patients that live at home or before they go home from rehab. Get them a sign that they can put up on their front door that can say, “Please wear your mask in my home and do your best to stay six feet apart.” It helps to do some of the communicating for them. We can also make sure that people have extra masks available because if somebody forgets their mask, they can then have a basket of them at the front door. There are a lot of places and organizations that are providing cloth masks for free. We have had hundreds of masks donated to Covell Care, which allows us to give them to patients and their family members. It is one less thing for them to worry about.
During treatment sessions, we can model social distancing as long as we are keeping a patient safe. I work with an occupational therapist who helps in the patient's kitchen. The only time she breaks the six-foot separation rule is when she needs to keep a patient safe from falls. In our current treatments, we can do them outside if the weather is nice enough. I have a patient that does the treatments outside because I also have students working with me, so I have to keep them separate from the patient.
Figure 10 is a picture of Gail with one of our patients, who is 94:

Figure 10. Gail treating a client outside.
There are some screening opportunities to do right now as well. For example, a co-worker normally does a circuit class in our facility’s gym. We cannot do that right now because the patients are not allowed to be in the gym. What we have done is taken it to the parking lot. She does her fitness class in three separate places around the building. Patients can come out on their patio and participate as long as they are safe. They can also participate in the parking lot. We strap a speaker to a desk chair and push it around the parking lot and she uses a megaphone.
How does that relate to us? I can go to those classes, and then be able to screen people by staying six feet away. We have been able to identify people that have had worsening conditions, even things that are not related to COVID that need to be addressed. I have also found that people are feeling depressed because they are socially isolated and need additional support services there. It can be very helpful to put eyes on the patients to make sure that they are doing well during this difficult time.
Strategies for Cognitive Impairments
Many healthcare professionals are working with older adults that have dementia or other cognitive impairments. That poses a lot of challenges for COVID-19. Some things that have been done in different memory care facilities and assisted living are using verbal cues and verbal signage. If directions are in big, bold print, it makes it easier.
I talked to an RN who works in a Colorado hospital. She said a lot of the patients that live in long-term care, memory units, or assisted living memory units, are experiencing more agitation and behaviors. Part of that is about the disconnect for human connection due to PPE. They also do not see any of their loved ones. This is a time to get involved because we can assess potential dementia-related behaviors that may be getting worse during the global pandemic. Some people are not being affected, but others are. We can train staff on how to reduce those behaviors and provide environmental training. This includes using music or lighting to help with those situations. You can also get creative with our activity departments and work to create social interactions while also social distancing. For example, we work in an assisted living facility that has a large kitchen, so they can congregate at one table to complete a task. What we have been able to do is modulate that out by having smaller groups. The folks that have cognitive impairments are positioned around the counters so they are not sitting right next to each other. Those are some of the contextual modifications you can do.
We also want to communicate concerns to providers. We know that a lot of patients are not reaching out to their physicians right now, especially if they are struggling with telemedicine, a lot of things are going unaddressed. If you know that your patient would have had a routine doctor's appointment but did not go because of COVID, do some assessments and get that information over to the providers. This prevents the situation from going unattended and promotes our importance with providers.
Figure 11 is a photo of a caregiver, who works with a person that has a mild cognitive impairment, and he goes with her out into the community.

Figure 11. Pin alerting people to stay "six feet away, please."
They both wear this button that says “six feet away, please.” It helps other people recognize the situation and take it more seriously for that person. Those are some ideas that you can do as well. I had a patient who would \wear a button that said, “I have low vision.” That way she was not struggling as much with judgment because it advocated for her.
Energy Conservation Training Post-COVID19
Fatigue and malaise are prominent factors for patients with COVID. We are seeing patients with mild cases of COVID getting better after about two weeks, but those with severe cases take six weeks or longer. Modulating that energy expenditure and making sure they are spending the energy where it is most effective is an important part of recovery.
On top of that, we are also seeing people become deconditioned because they have been so socially isolated. They are not engaged in as many activities, not getting up as much, watching more TV, and are more sedentary. We have to address energy conservation and recovery, even with patients that do not have COVID-19. We want to advocate for our treatment in situations like these because our providers do not always understand. Advocate for your providers about what you can do related to COVID. We know that patients with comorbidities are going to take longer.
Community Mobility Training
Did you know that places like grocery stores are removing benches and tables? It is to reduce the risk of crowds gathering. However, a patient could tell me that they want to take a break, but the benches and tables are gone. We now have patients that are struggling to just get out in the community and do their normal shopping. It is a good idea to ask your older adult patients if they have been to the store, and then ask if they have noticed any changes that would affect them. If they have not been back to the store, it might be a good idea to ask a family member to go to the store and check it out.
Make sure chairs are still there, because if they are not you may have a patient in trouble. The patient may need a four-wheeled walker for outings. This is because if there are benches, we do not necessarily know they will be there the next week. They are unanticipated changes that people are not expecting.
We talked about doing a training on infection prevention when in public. We can also work on ordering groceries online for pickup or delivery. I also know for our older adults that increased ordering online is going to reduce the need to have to go out into the community. It would also be helpful to tap into social connections virtually. If they are used to going out in the community, we can talk to them about messaging other people to join via your computer. If they do not know how to do that, we can teach them.
Address Caregiver Burnout
We have to be considering patients’ caregivers during treatment planning. This is because if a caregiver is overwhelmed, then not only is our patient at risk; the caregiver is as well. During COVID many families have had their lives turned upside down, and that includes both personal and professional caregivers. We have families that have had to pull loved ones out of nursing homes to reduce the risk of COVID. Others work in independent and assisted living. Adult Day programs are closed as well, so that is a sudden loss of support. They may have kids at home and doing homeschooling on top of being a caregiver. Now that it is summertime, kids are likely going to be home more. Camps are canceled, as well as other activities that they normally rely on for support.
Caregiver burnout risk is at an all-time high for older adults, and all health professionals have to consider this in their profiles for their patients. You can start considering that wherever, whether you work in the hospital, home care, or long-term care. If a caregiver is showing signs of burnout, such as tearfulness, statements of feeling overwhelmed, being too quick to get irritated, your radar should start to go up. I encourage everybody to find a caregiver burnout assessment. You can do a quick run-through, or even do a self-reporting questionnaire. While seeing the patient you can say, “While I do treatment with your mom today, do you mind filling out this form for me and giving it to me at the end of treatment?” It also gives you ideas about which areas they may need support in.
We have to start looking at this, especially when it comes to COVID. This is because everybody is on top of each other and there has been just a lot of strain and stress across the board. For example, I had a patient who had dementia and Parkinson's disease and was a professor at a university before she retired. She was always working at local community events. As she got sicker, she had professional caregivers coming in to take care of her. They were doing a great job, but I noticed that she was not engaging in the activities, and she became agitated towards dinnertime. The caregiver would put her in her comfy chair, put her feet up, give her a blanket, and turn on a show, which sounds like something we would all like to do. However, she would get more agitated and she started saying nasty things to the caregiver, which led to caregiver burnout. I suggested she take the caregiver to the kitchen to see if we could get her engaged. We put her at the counter and we started giving her tasks to do every day, such as putting vegetables into the salad or making a cookie tray for the table. These simple tasks helped her agitation level come down, so she was then more cooperative for bed and the caregiver had less strain.
There are different ways that we can look at how to manipulate people's routines that can support the caregiver and their overall well-being, while also supporting our patient. If your caregiver is showing signs of burnout, make sure that you know resources in your community or what your agency is recommending. If it means bringing in more non-medical care providers during COVID, is that safe? You have to be able to have those conversations with people. If you have a counselor or social worker on your team, I encourage you to refer to them and they will be able to support your plan, as well as the caregivers’ and patients’ mental health.
Improve Social Connection
We can incorporate social connections into treatment plans as well. If you have a patient in the hospital or in rehab, think about bringing a patient's family member into the visit virtually. Even if they are not willing to use technology, you have probably got a computer or device. Even if they wanted to show what they did during treatment, bring that into the treatment plan and have them engage. Socialization is key right now for a lot of our older adults.
Focus on the therapeutic use of self. Think of ways that you can improve that social connection. If you are coming in and you see something pretty, take a picture of it and show them that way. I have done that for patients who are homebound. If their flowers are growing outside and they cannot get out and see them, I have taken pictures of them and showed them when I come into the house. Be mindful that 12 million Americans over the age of 65 are alone. If you work in-home care, know that you might be the only one that the person is going to see. This is because family and neighbors are not stopping by as much. Take the time, focus on the therapeutic use of self, and train patients on technology options to increase socialization. That can be in your treatment plan and can be made into measurable goals.
Figure 12 is an image of a patient and her chickens.

Figure 12. A client and her chickens.
This is a telehealth visit. We started talking about what she does during the day and what brings her joy. She said, “I'll be right back.” She went, got her little chickens and introduced them to me via telehealth. It is all about the therapeutic use of self, and I felt good when we both left that visit. Make sure you are putting your heart into your visits.
Expand Feelings of Purpose
Going online with socialization and connection can expand feelings of purpose. We also need to help patients feel like they are contributing some way. They can write a letter to somebody or help a meaningful project, which helps them identify things to look forward to.
I once had a patient in a skilled nursing facility tell me that life is over when you no longer have something to look forward to. Right now, there are a lot of things they cannot do. They cannot go to graduation ceremonies, or weddings, etc. Events are getting canceled. What can they look forward to? What can they participate in? Dive into that to help them manage on their own because they are not having as much support as they used to. Their family members may still be coming over to visit as often, but they also may be overtaxed due to their own lives right now. You can help them with things to get them engaged and look at what they can do to help. Getting people engaged is key and we need to start doing that while people are isolated.
Promote Comprehensive Self-Care Routines
We can help patients establish positive self-care with routine exercise, getting outside, and making sure that they are initiating some socialization, even if it is just a phone call. We can do that with ch

