Editor's Note: This text is a transcript of the course Environmental Modifications for Adults with Low Vision presented by Monique Chabot, OTD, OTR/L, SCEM, CLIPP, CAPS.
Learning Outcomes
After this course, participants will be able to:
- Describe supports and barriers faced by adults with low vision within their environments that impact participation and communication.
- Identify intervention ideas that are appropriate for their clients, including low-cost modifications, lighting, contrast, and smart technologies.
- Describe how to integrate assessment and environmental modification interventions to improve communication and overall participation.
Introduction
As mentioned, this course is "Environmental Modifications for Adults with Low Vision." While our discussion primarily focuses on adults in general, it's common to encounter older adults with low vision. Therefore, I strive to maintain a balanced approach throughout our conversations, addressing both demographics.
Before entering academia, my clinical background primarily involved geriatric house calls. Working within a MobileMed B practice, I've predominantly served older adults throughout my career, gaining extensive experience in various home environments to support daily participation. This has exposed me to diverse situations and challenges, enabling me to effectively assist individuals. Additionally, I've had the privilege of collaborating with excellent SLPs, and continue to do so at Widener University. We work together in our pro bono clinic and coursework, fostering mutual learning and growth. I'm excited to share my knowledge and engage in further discussion with all of you on this topic.
Statistics
In terms of low vision prevalence in the US, as of 2016, it's estimated that approximately 7 million individuals are affected by some form of vision impairment. Looking ahead, projections indicate that the number of people considered legally blind is anticipated to surpass 8 million by 2025. This increase is largely attributed to the growing population of older adults, a demographic expected to undergo significant expansion in the near future, often referred to as the "silver tsunami." Given the strong correlation between age and low vision, this demographic shift is expected to contribute substantially to the rise in cases.
Currently, the primary causes of vision loss in the US are cataracts, closely followed by glaucoma. However, in my general practice, I frequently encounter individuals affected by the conditions we'll be discussing.
SLP and Low Vision
Concerning speech therapy and low vision, there was a study conducted in 2020 that shed light on the challenges presented in treatment. Specifically, individuals with low vision face obstacles in various aspects of therapy. For instance, visually locating food during feeding activities poses difficulties, making it difficult to continue the task of eating. Also, navigating communication devices can be challenging due to vision impairments. Additionally, interpreting nonverbal communication becomes problematic, as individuals may struggle to process and respond to these cues effectively. Lastly, completing exercises that rely on visual feedback may prove challenging for individuals with low vision.
Low vision has been observed to affect various communication skills, potentially impacting language acquisition and different interaction abilities, particularly the nonverbal component. It may also hinder interpersonal relationship building and pose challenges for alternative communication methods. Consequently, individuals with low vision may find it difficult to use sign language and other communication options, leading to a lack of focused attention on a speaker. This is often seen in certain conditions where it's unclear if someone is looking directly at the speaker due to their visual field limitations. Without awareness of that, it may appear as though the person is not paying attention.
Impact of Environmental Modifications
We know that environmental modifications can play a key role in supporting participation in activities of daily living, and vision impairments do significantly decrease participation. The literature predominantly emphasizes fall prevention and lighting as primary concerns across disciplines when addressing low vision in environmental contexts. This focus stems from the concern over home accidents and the adverse health effects they can have.
Thus, the literature extensively discusses lighting and contrast, which we will discuss in detail shortly. These modifications help individuals familiarize themselves with tasks and environments so that they are more predictable and reduce the need to rely on vision to complete the task. Additionally, organizational strategies and enhancing the visual accessibility of tablets and video communication platforms are highlighted. These adjustments not only increase independence but also facilitate social connectivity and provide more communication opportunities.
I also want to mention that a systematic review found no significant evidence favoring environmental modifications or behavioral interventions in aiding individuals with low vision in their daily lives. However, the review highlighted the poor methodologies and outcome measurements in the studies, indicating a lack of definitive conclusions. Therefore, a combination of both environmental modifications and behavioral interventions is key for assisting individuals with low vision in their home or living situations.
Low Vision Overview
Let's look at the various conditions we're discussing. First, low vision is a condition caused by a disease. It is characterized by a visual acuity of 20/70 or lower in the better eye, which cannot be improved through medical or surgical interventions or eyeglasses. For example, although I wear glasses and have lower visual acuity, I'm not classified as having low vision because my vision can be corrected to 20/20. However, individuals characterized with low vision cannot achieve this level of correction and can only be corrected up to 20/70. It's important to note that having low vision doesn't imply a complete inability to see, which is a common misconception. Total blindness is not necessarily low vision, as many individuals with low vision can still see various aspects of their environment.
Legally blind is defined as having a visual acuity of 20/200 or less in the best-corrected eye or a visual field of about 20 degrees or less in the better eye. To put this into perspective, imagine your shoulder represents approximately 90 degrees of visual field. Halfway toward the center would be about 45 degrees, and then coming in further, about 20 degrees would be around this area. Individuals with a visual field of 20 degrees or less can't see anything beyond that 20-degree point. It's important to understand that at 20/200, individuals can still perceive light and distinguish various objects. It doesn't mean total blindness.
What that means for reading or near-to-normal vision, it typically ranges from 20/20 to 20/60. You may require reading glasses or need to hold things closer to read, but reading is still feasible.
From low vision to being classified as legally blind, the spectrum extends up to 20/1000. At 20/80, magnifiers become necessary, and contrast is critical for distinguishing objects. Facial expressions may also become challenging to interpret at this level. Around 20/60, it's generally recommended to cease driving. As visual acuity decreases to 20/200, performing various tasks and maintaining mobility becomes increasingly difficult, as there's a higher risk of collisions or tripping. At 20/500, reading continuous text is difficult due to the significant need for magnification, which makes it challenging to see the full text in order to scan and read. Near-total blindness is typically characterized by visual acuity ranging from 20/1250 to no light perception, at which point vision is considered unreliable or nonexistent.
Common Diagnoses
Let's explore various diagnoses, including cataracts, glaucoma, macular degeneration, and diabetic retinopathy, and touch upon age-related changes in vision. These age-related changes are universal and may affect all of us, provided we live long enough. Each diagnosis comes with its own set of causes, symptoms, and lighting preferences. As we progress through the content, you'll notice that I've organized it to include information on the causes, treatment options, functional impacts, individuals' sensitivity to light, and their preferred lighting levels to facilitate their activities.
Cataracts. Cataracts are the most prevalent cause of low vision in the US. Cataracts occur when the lens of the eye becomes cloudy. Surgical intervention involves removing the affected lens and replacing it. Often, the replacement lens corrects visual acuity, reducing the need for glasses, particularly for near and far vision, with reading glasses being sufficient. However, cataract surgery can result in blurred vision, difficulty in discerning objects with low contrast, and reduced color discrimination, particularly in blues and purples, due to the cloudy lens imparting a bluish or purplish tint.
Given these challenges, it's best for individuals with cataracts to avoid using colors that resemble blues or purples. Moreover, they often experience heightened sensitivity to glare, impacting activities such as reading, watching TV, and driving. While they are sensitive to light, they also prefer higher levels of illumination to compensate for the clouding in the lens and facilitate better visibility.
Glaucoma. Moving on to glaucoma, the second leading cause of low vision involves high intraocular pressure exerting pressure on the optic disc or nerve. Various factors, including scar tissue, surgical procedures, eye changes, and genetics, can contribute to this condition. When visiting the optometrist's office, they typically assess intraocular pressure, often using a puff of air, to screen for glaucoma. Individuals with a family history of glaucoma undergo a thorough evaluation to ensure early detection and appropriate management.
Glaucoma is typically managed with eyedrops, although surgery may be necessary in some cases. However, despite management efforts, it often results in tunnel vision, wherein peripheral vision gradually diminishes, resembling the sensation of looking through a narrow tunnel. This reduction in peripheral vision poses challenges in navigating surroundings, as individuals may inadvertently bump into objects due to their limited visual field. Without proper management, glaucoma can progress to blindness or result in scotomas, which are blind spots in the central vision. Individuals with glaucoma tend to have moderate sensitivity to light and prefer a moderate amount of light. While they don't require as much light to penetrate through cloudy lenses as in the case of cataracts, they still need adequate lighting to compensate for the loss of visual field and make out their surroundings effectively.
Macular Degeneration. Macular degeneration is the destruction of the cells in the macula and manifests in two primary forms: wet and dry. In dry macular degeneration, which constitutes around 90% of cases, there is typically unilateral involvement characterized by cell atrophy in the macula. Certain vitamins can be taken to decelerate its progression. Conversely, wet macular degeneration, accounting for about 10% of cases, tends to be bilateral and more aggressive, leading to rapid vision loss. It is often associated with a genetic component and results from blood vessel rupture. In cases of wet macular degeneration, individuals may require injections to stop the hemorrhaging and preserve vision.
Macular degeneration affects the central field of vision, making tasks requiring fine details, such as reading and facial recognition, particularly challenging. Since the macula is located in the middle of the eye, individuals with macular degeneration experience difficulties with central vision. To compensate, they may need to rely on their peripheral vision, which remains unaffected by scotomas (i.e., blind spots). This may result in individuals appearing to look slightly away while engaging with others as they use the unaffected parts of their vision. They typically have heightened light sensitivity and prefer a bright light. We'll look at the qualities of light later on, but it's important to note that while they don't necessarily require a high level of light, they do need it to be bright and of a specific color.
Diabetic Retinopathy. Diabetic retinopathy, as the name suggests, is a complication of chronic diabetes resulting from elevated blood sugar levels. In this condition, the blood vessels in the eye are damaged, leading to leakage of lipids and fluids onto the retina. This can result in oxygen deprivation and various other eye-related issues. Hemorrhaging also contributes to the development of scotomas, or blind spots. Treatment often involves injections, but effective management of diabetes is crucial. Interestingly, the severity of retinopathy in individuals with diabetes tends to fluctuate based on their blood sugar levels. Therefore, better control of blood sugar can lead to improved eye health on certain days.
Scotomas, or blind spots, in individuals with diabetic retinopathy, can shift depending on the location of blood spots on any given day, making the condition highly unpredictable. Visual field loss and sensitivity to glare are common symptoms. Some individuals may experience reduced visual fields, with the extent of deficits varying based on individual presentations. They typically have moderate sensitivity to light and prefer a moderate level of light. I have only had a few clients with diabetic retinopathy. However, their cases were so advanced that one gentleman actually lived in a completely dark basement because that was all he could tolerate.
Age-Related Vision Changes. As we age, we inevitably experience age-related vision changes, which are inherent to the aging process. These changes commonly include difficulty in near vision, challenges in color discrimination, and a natural yellowing of the lens of the eye. Consequently, colors such as yellow, blues, and purples may become difficult to discern, especially when compounded with conditions like cataracts. Additionally, weakening muscles in the eyes can lead to difficulties in adjusting to varying levels of light. Moreover, decreasing visual acuity is a common occurrence. These adjustments often prompt individuals to opt for progressive lenses to address these age-related vision needs.
Assessment
Identified Concerns for Low Vision
Research has examined various home assessments to determine their efficacy in evaluating lighting conditions. Interestingly, many of these assessments aren't specifically tailored for occupational therapists (OTs) but are designed for use by multiple professionals working in home environments. What researchers found is that no single home assessment comprehensively addresses lighting concerns. While some assessments may differentiate between indoor and outdoor lighting or discuss contrast, others may simply provide a single-line assessment such as "adequate light," which can have different interpretations.
When evaluating a person's environment, certain key areas of concern are worth considering in terms of how they interact with the individual. Adequate lighting in critical areas such as storage spaces under cabinets, task areas, overhead lighting, outdoor spaces, and the ability to adjust windows for natural light are all significant factors to assess.
Ensuring adequate contrast in key areas, particularly for functional mobility, is essential. Much of the literature emphasizes concerns about falls, making contrast an important factor to address. Visual distractions, such as patterns on countertops and furnishings, as well as clutter, can interact with a person's visual processing and create difficulties. Glare poses another significant challenge. Sources of glare can cause discomfort, reminiscent of the sensation experienced when a camera flash goes off directly in the eye, and can persistently disrupt vision. Additionally, individuals may encounter difficulties in adjusting to varying light levels, which can be problematic. Providing support for compensatory strategies is important, as individuals often rely on these strategies to navigate their daily lives effectively despite visual impairments.
Individuals with visual impairments often utilize a variety of compensatory strategies, including sensory cues such as touch and sound, cognitive strategies, and familiarity with their environment to navigate effectively. It's critical to ensure that environmental factors do not hinder the effectiveness of these strategies. Assessing factors such as the readability of fine print on appliances and remote controls, as well as the accessibility of electronic devices, is important in promoting independence and functionality. As a reminder, combining both environmental modifications and behavioral interventions is essential for effective support and adaptation to visual impairments.
Home Assessment: HELA
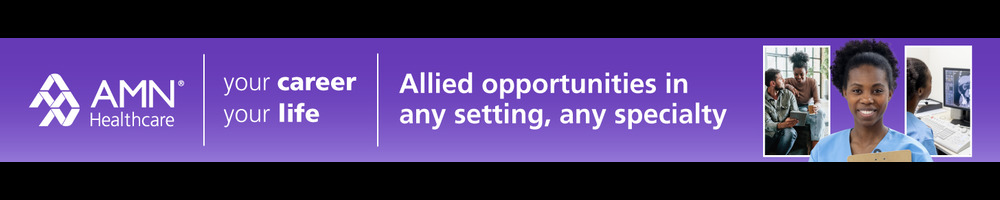
Two specific assessments focus on lighting and the environment, which could be valuable tools for structuring your approach to addressing the situation you're treating. The first assessment is known as HELA, which stands for Home Environment Lighting Assessment. It comprises four main components (see Figure 1). Initially, it involves describing the environment and obtaining light readings to assess the current lighting situation. This includes examining the number and type of bulbs used, as well as their wattage.
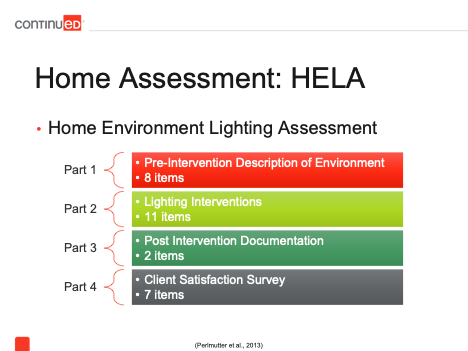
Figure 1. Home Environment Lighting Assessment.
Additionally, we use the MinnesotaRead assessment (MNRead assessment), which focuses on evaluating an individual's reading abilities, particularly at close distances. This assessment provides specific insights into acuity levels and identifies any issues related to glare or the need for item repositioning. Following the assessment, a structured lighting intervention is given that offers 11 options for improvement. These options range from adjusting wattage and bulb type to adding lampshades or lighting sources as necessary.
Following the lighting intervention, the MinnesotaRead assessment is repeated, and light meter readings are documented to assess any improvements. Additionally, a client satisfaction survey is administered to see how they like the changes that were made. It's important to note that lighting preferences and needs vary greatly among individuals with low vision, emphasizing the importance of obtaining feedback on satisfaction with the intervention. One specific question that is good to ask is whether or not they are using the intervention, and if they're not, why not?
Home Assessment: HEAVI
Another assessment worth considering is the HEAVI, which stands for Home Environment Assessment for the Visually Impaired. While primarily designed for fall prevention, it also addresses specific visual concerns. This assessment offers a different perspective on evaluating the environment, whether you're in a clinic or a home setting, to observe how the individual interacts visually with their surroundings. By incorporating suggestions from the assessment into your treatment approach, you can enhance the overall care provided. The HEAVI assessment examines various rooms and characteristics of the home, identifying potential fall hazards. Interestingly, the assessment identified 119 unique fall hazards that could be addressed. It covers aspects such as floor glare, contrast, and safety features to comprehensively address visual and safety concerns.
Other Areas to Address
There are also some other areas that should be addressed. First, we need to ensure access to light while mitigating glare, which is a major concern. It's important to provide access to light without introducing more glare into the environment. Additionally, we emphasize the importance of adjustable opportunities in architecture, allowing individuals to adapt their surroundings to meet their needs effectively. This is most obvious in features such as adjustable blinds and curtains to control the amount of light entering a room. Being able to adjust blinds or curtains to block light or let more light in is considered an adjustable opportunity.
Smart light bulbs also offer versatile options, allowing users to adjust brightness, color, and even schedule lighting preferences through a single app. Ensuring access to outlets and switches in convenient locations is critical, minimizing the need for extension cords that can create trip hazards. Furthermore, it's essential to position lights closer to task areas to optimize visibility and functionality.
Another aspect we need to consider is participation support. This involves evaluating whether the assistive devices being used are suitable choices for the individual. Some devices offer more accessibility features that may be better suited for individuals with low vision. We want to assess how the items we've introduced interact with the environment in terms of clutter and visual distractions. For example, the color of countertops or other elements in the environment can impact the visibility of certain items. We'll explore examples of visual distractions and clutter to illustrate this further. Making informed choices based on these considerations can greatly enhance the individual's ability to navigate their environment effectively.
Is there sufficient contrast to support the identification of items or interactions with different objects in the environment? Additionally, we must consider the characteristics of print materials, including factors such as color, size, and font. While larger print may seem beneficial, it's important to strike a balance, as excessively large text can impact the ability to read continuous text. Conversely, text that is too small may be difficult to read. It's important that print materials are sized appropriately to maintain readability without obstructing other forms of environmental support, such as compensatory strategies involving other senses or cognitive strategies.
Tools of the Trade
Light Meter. In my practice, I often use tools such as a light meter, as shown in the handheld device in Figure 2. Additionally, I rely on a mobile app on my phone, allowing me to promptly assess the level of light in any given space. Numerous free apps are readily available for download that can measure the brightness of light, typically indicated in lumens.

Figure 2. Light meter.
Vision Assessments. In addition to light assessments, there are various vision assessments available. The MNRead assessment, as mentioned earlier, is one commonly used tool. Another is the Schell Chart, which involves standing 20 feet away and reading the smallest line, available in different formats, including letters, numbers, and symbols to accommodate various literacy and cognitive needs. Additionally, the LEA Contrast Sensitivity Chart is used, resembling a flip book with varying levels of contrast for the same words, allowing for the assessment of an individual's sensitivity to different color contrasts.
Typical Tools. I also bring along a tape measure, a picture-taking device, and a notebook, among other tools. These items help me create a floor plan, measure distances, and keep track of important details during assessments.
Environmental Modification Interventions
Contrast
When considering environmental modification interventions, contrast is a key feature in home settings. It serves multiple purposes, including acting as a marker for household organization. For instance, using different colors as edges on shelves can aid in distinguishing between items and their surroundings. Additionally, contrast can be used as a warning for potential hazards. For instance, I often use tape around cabinet doors; if a door remains open, the tape serves as a visual cue that alerts the person that the door is still open.
I've also used contrast to mark specific locations for essential items. For instance, I designate a spot for keys using bright lime green duct tape, making them easy to find. Maintaining a sufficient level of contrast is essential in these instances. Neon green duct tape, in particular, stands out effectively for individuals with low vision and can also benefit those with dementia. While certain shades of red may also be effective, I've found the neon green color to be most successful in my experience.
Also, contrast can extend beyond color and include variations in shape or texture to enhance visibility and accessibility for individuals with visual impairments or cognitive challenges. For example, adding a specific sticker to containers used for thickening liquids or powders allows individuals to feel where the line should be or identify the container more easily. These tactile cues can help with gathering necessary items. As previously mentioned, duct tape, particularly neon green, is one of my preferred interventions, and I always carry a roll with me. Additionally, foam stickers found at craft stores are another useful tool for providing contrast and tactile feedback in the environment.
Additionally, commercially available raised plastic dots and "tactile markers" (i.e., puffy paint) are useful resources for enhancing tactile feedback in the environment. Alternatively, you can use materials like puffy paint or foam stickers, although they may not be as durable as their commercial counterparts. These budget-friendly options are suitable for quick interventions. Another strategy is to cover busy countertops with plain placemats to increase contrast, reduce visual distractions, and help the person focus and process what they are looking at.
Additionally, contrasting colors can be applied to the inside of cabinets to show that the door is open or to differentiate between items stored within the cabinet, particularly when using containers with similar colors to the cabinet. Changing the backdrop color to a darker or contrasting hue can make containers stand out more, helping individuals locate items necessary for their tasks.
Additionally, increasing lighting levels enhances visibility in the environment. Another helpful strategy is the use of signature and writing guides, such as the one depicted in Figure 3. These guides, available in various sizes and commercially purchasable, provide structured support for writing tasks. They are available in sizes suitable for checks, credit cards, and even full-page templates, including envelopes. Additionally, these guides serve as valuable cognitive support, assisting individuals in organizing their thoughts and actions effectively.

Figure 3. Writing guide.
Figure 4 (image on the left) is a photo taken at my grandparent's house. You can see that I added bright red electrical tape around a white cabinet that is very close to the toilet. My grandmother was 4'11" tall and had vision challenges, so I applied tape to areas where she might inadvertently hit her head. Interestingly, my grandfather didn't want the tape there because you could see it. I explained to him that was the intent, to serve as a visual cue to prevent accidents—an approach that ultimately proved effective. Additionally, I added tape to the ends of window poles to help my grandmother find them when she wanted to adjust the lights.
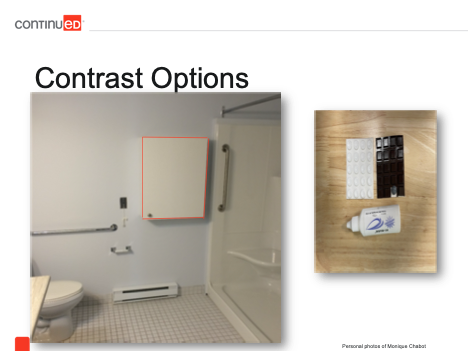
Figure 4. Contrast options.
Figure 5 shows a bottle of tactile marker, similar to paint, used to make dots to mark off an area or create designs to mark different tools for clients to use in a treatment session. The plastic dots in Figure 5 are an example of what can be purchased commercially.

Figure 5. Tactile contrast tools.
When considering contrast, we want to consider the light reflectance value (LRV), which is often found on the back of paint chip strips. While LRV values are commonly associated with paint colors, they are applicable to any color.
LRV measures the amount of light a color reflects, ranging from 0% for darker colors that absorb all light to 100% for lighter colors that reflect all light. Ideally, there should be a significant difference between LRV values, ideally at least a 20% contrast. While some paint chips may display LRV values, others may not; however, each increment typically represents a 10% difference. Therefore, aiming for a 20-point difference between two colors is advisable. Lighter colors generally have a higher LRV than darker ones, with white causing more glare compared to yellow or other colors.
Lighting
When discussing lighting, clients often say the lighting in their homes is poor but are apt to dismiss the issue. However, this is typically due to a lack of education about lighting options and their potential to improve daily life. To address this, I've occasionally used my phone flashlight under a cabinet to show the improvement, and then clients recognize the difference better lighting can make. To determine the most effective lighting solutions, it's essential to conduct a comprehensive and personalized assessment of the lighting situation.
Lumens. If you search online, you can easily find recommendations for the appropriate lumens for different spaces. Lumens measure the brightness of light, and every room has a recommended amount of lumens. However, in many cases, the actual lighting is well under these recommendations, except perhaps in more commercial settings. The recommended lumens tend to be higher in areas with more activity or where increased energy is needed. For example, kitchens typically have a higher lumen rate compared to bedrooms, bathrooms, or offices. You can find specific recommendations online. So, what we can do is take one of those recommended numbers and divide it by the number of outlets in the room. This calculation gives us an idea of how much illumination each light fixture should have to meet the recommended lumens for the space.
Kelvin. Kelvin refers to the color of the light. For instance, you might notice a slight yellowish tint in my video because I prefer the warmer spectrum of light bulbs due to personal light sensitivities. Essentially, the cooler the light, the more bluish or cool it appears to us. Higher Kelvin ratings indicate a daylight or bluer light, such as the blue light emitted from our phones. This is considered a hotter light. A simple way to remember it is to think of a flame— the middle part, which is blue, is hotter. We can adjust the color of the light, and different people react differently to it. Generally, people tend to prefer cooler color lights, finding them more comfortable, especially those with low vision.
Wattage. When it comes to wattage, it refers to the amount of power handled by the outlet. Nowadays, most light bulbs are LEDs, and you'll often see on the package that they're equivalent to a certain wattage, like a 40-watt bulb. This is because we used to rely on incandescent bulbs, so we still have that mental image of what a 40-watt light looks like. However, the brightness of a bulb is actually measured in lumens, not wattage. Despite this, people often associate wattage with brightness. With LEDs and other energy-efficient bulbs, we can achieve much higher brightness levels with lower wattages. For example, an LDE bulb labeled as equivalent to a 40-watt incandescent bulb might only use around eight watts of power. So even though it's labeled as 40 watts, it will provide much more light than the old incandescent bulb. This is an important point to explain to clients who may still be accustomed to the old incandescent bulbs.
Individual Sensitivity. Individual sensitivity varies greatly when it comes to lighting. What works well for one person might not suit another at all. There's a multitude of factors influencing our reaction to light, spanning cognitive, emotional, and physical aspects, in addition to the variation caused by different eye conditions. Even among individuals with the same eye condition, sensitivities and preferences can vary widely. In the past, we used to resort to trial and error, testing out different light bulbs to find the right fit. However, with the advent of smart bulbs, the process has become much more streamlined. Now, I can simply install a smart bulb, use the accompanying app on my phone, and fine-tune the brightness and color temperature (i.e., lumen and kelvin settings) to meet the specific needs of the individual—all from a single bulb.
Lighting Interventions
Certainly, there are various options available for lighting solutions, depending on the specific needs of the individual. For instance, the light in my linen closet is mounted on the wall, providing a permanent and reliable source of light. However, there are also battery-operated puck lights that offer flexibility and convenience. These lights come in different configurations, including options with rechargeable batteries, which can be more cost-effective and environmentally friendly in the long run. Some puck lights are designed to be mounted onto the wall with screws, while others feature adhesive backing for easy installation. Additionally, these lights come in a range of brightness levels and colors, including nightlight options that emit softer, warmer light which are ideal for our clients who wake in the middle of the night and we don't want to disturb sleep.
When using adhesive-backed lights such as puck lights, it's common for the adhesive to be less durable over time. To address this issue, I replace the adhesive with a more reliable option, such as 3M stickers, to ensure the lights stay securely in place. For example, I've personally applied a sturdy 3M sticker under my cabinet where I engage in various tasks like 3D printing and soldering for my assistive technology work. It's a quick and easy installation and allows me to control the lighting on my countertop, including options to adjust color, brightness, and other settings using a remote control.
I've used both motion-sensored and tap-controlled lights in different areas of my home. For instance, the light in my linen closet is motion-sensored and automatically turns on when the door is opened. These lights come in various shapes, sizes, and brightness levels to suit different needs. Additionally, there are options for task lighting using rope lights or bar lights, such as the one I have installed under my counter. These lights can be activated in different ways, including motion sensing.
Sometimes the simplest solution can make a significant difference. I often find that just changing the light bulb to one with higher lumens while still staying within the wattage limit of the fixture can have a remarkable impact on the brightness and overall illumination of a space. Additionally, adding lamps throughout a room can help to distribute light more evenly, providing better coverage and reducing shadows.
When it comes to selecting light bulbs, hardware stores typically offer a variety of options displayed on shelves or in dedicated sections. These displays showcase different types of light bulbs, including those with varying levels of brightness, color temperatures, and energy efficiency. By choosing the right combination of bulbs for a space, we can effectively tailor the lighting to meet the specific needs and preferences of the individual.
Light Bulbs
Natural/Daylight. Looking at Figure 6, on the far right-hand side is the natural daylight bulb. It's basically the same as natural light from outside and is often considered one of the best sources of illumination for various activities. It provides a neutral light that allows people to perceive colors accurately. However, it also has a tendency to cause glares, shadows, and harshness in some individuals' eyes. While we do test it, we typically don't rely heavily on natural light except for general, big-level lighting interventions.
Figure 6. Light bulb options.
Soft-White CFL. Soft white light, which closely resembles traditional incandescent bulbs, is located on the opposite end of the spectrum. Soft white light offers a warmer ambiance with less glare due to its more yellowish hue, making it a preferred choice for many, including myself. However, the lighting has to be set up carefully to avoid creating sharp shadows, which can cause difficulty processing the environment and even trigger hallucinations for some individuals. So, we use it strategically and carefully. Additionally, we want to be sure that the placement of soft white light doesn't obscure important items or tasks on countertops or other surfaces.
Bright-White. Bright white light, which is between soft white and natural daylight on the spectrum, is typically preferred for task lighting, such as desk lamps, as it offers a softer illumination compared to natural daylight. Unlike soft white, bright white light doesn't create pronounced shadows, making it more tolerable for many individuals. However, it may still cause glare on glossy surfaces, so we may need to adjust the lighting setup to minimize glare effects. Fluorescent lights are often bright-white light, but they also tend to flicker, which can be problematic, particularly for those with low vision issues. Warm white light falls somewhere in between soft-white and bright-white light.
While individuals have varying sensitivities and preferences, understanding these differences is a good starting point when determining the appropriate lighting for a given scenario.
Visual Distractions
When we talk about visual distractions, we're referring to reducing clutter. I won't show you what's happening with my desk because it's the complete opposite of what an environment free of visual distractions should be. Essentially, people use their countertops to store all sorts of things. If you can't find something, it usually ends up on the countertop, and by minimizing clutter, it becomes easier to locate items.
We want to avoid busy patterns on items like tiles, couches, and bedspreads. Small polka dots or pinstripes, in particular, tend to cause visual distortions, which can be quite unsettling. In such cases, we may cover troublesome patterns with plain color blankets or use placemats to reduce visual overload. Additionally, using plain placemats can help with locating items, especially if they offer good contrast. Simply labeling containers and bins, as well as reorganizing items, can also be effective strategies. Also, considering aspects of cognition plays a significant role in implementing compensatory strategies to help people navigate their environments effectively.
Visual Distraction Intervention. This is my countertop in the kitchen (Figure 7). I must admit, I didn't pick this countertop; it came with the house.
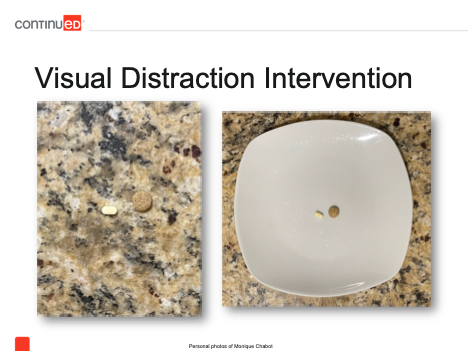
Figure 7. Visual distraction - busy countertop.
However, as you can probably imagine, on most mornings, I struggle to spot my vitamins on the left-hand side because they blend right in. But when I place a plate underneath them, suddenly, I can see my vitamins clearly. I've applied this intervention for various individuals facing similar challenges where items they need to interact with or manipulate become hard to see due to the countertop's design.
Glare
Diffuse Light. Glare is a huge concern because of how it reflects into the eye, creating sharp, shiny spots that people struggle to adjust to. The initial step is to diffuse the light. If there are multiple concentrated spots of light, it intensifies the glare because of the high contrast between light and dark. By incorporating multiple small sources of light, we can disperse the light more evenly. Additionally, using lampshades or covers on bulbs softens the light and reduces glare. Window treatments are also effective, as is increasing the overall brightness around the glare source.
At certain times of the year, I have glare issues due to sunlight streaming in. To mitigate this, I turn on my overhead light and another lamp on my desk corner. This helps minimize the sharp contrast between the incoming sunlight and the overall room environment, reducing glare. Additionally, it's recommended to use two light sources on the opposite side of the room when natural light enters through a window, further diffusing the light and counteracting glare.
Light Quality. So, while we focus on increasing brightness (increasing the lumens), it's important not to overdo it, as excessive brightness can lead to glare. If someone experiences glare from a light source, consider slightly reducing its intensity. Additionally, adjusting the color of the light towards the warmer, yellow-orange spectrum can alleviate glare. Maintaining the overall room lighting at recommended levels, which can be easily found, is important. And having adjustable lighting controls, such as dimmer switches, is invaluable for optimizing lighting conditions. Smart bulbs also provide this option.
So, when arranging workstations, windows and light sources should be aligned parallel to the line of sight. In my office, this setup is generally effective, but when the sun shifts position, it can create a scenario where light enters perpendicular to the line of sight, causing glare. This is problematic because we want to avoid directing light directly into people's eyes. Additionally, it's best to avoid placing light sources directly overhead or in front of the workstation. Instead, positioning lamps to the side helps prevent glare and ensures that light does not bounce off at an angle that can affect visibility.
When selecting material finishes, it's preferable to opt for matte surfaces on tables, countertops, and even tiles. Shiny finishes tend to reflect light, which can cause glare. Additionally, you can adjust paint finishes to be flat or semi-gloss, as some individuals are highly sensitive to glossy surfaces, whether it's on countertops or walls. It's also important to consider the type of paper used, as low gloss paper can significantly reduce glare. Conversely, high gloss paper or lamination, while durable, can create unwanted reflections due to its shiny surface.
When it comes to paper products, opting for matte finishes, such as matte page protectors, can help minimize glare compared to glossy finishes. This is an important consideration. Regarding smart technologies, there's substantial evidence supporting their role in preserving independence and autonomy among individuals with vision impairments. Additionally, these technologies can be valuable tools for enhancing cognitive abilities and compensating for cognitive challenges, although delving into this topic would require a separate course.
Smart Technologies
When considering smart technologies, particularly for individuals with low vision, some individuals may experience dual sensory loss, involving both decreased vision and hearing. This influences the types of cues that are most effective. Generally, individuals prefer verbal or auditory cues initially, followed by vibration feedback, if they only have low vision. However, if someone also has hearing loss, verbal or auditory cues may not be suitable, necessitating the use of vibration options.
We also need to examine the control mechanisms. Are there options to adjust the font size in the app, enhance contrast on the controlling device for smart devices, and reduce glare on screens? It's important to have variable control options for individuals unable to use touchscreens due to accessibility concerns, as touchscreens lack tactile feedback. While verbal control may allow navigation of smartphone apps, if the app lacks accessibility options, the smart device won't function well.
Additionally, it's beneficial if smart technology offers automation routines. For instance, many smart light bulbs can be programmed to turn on and off at specific times of the day. Even if the app lacks verbal control or settings adjustments for better visibility, automation routines can help mitigate some of the issues.
Smartphones and Tablets
Smartphones are increasingly replacing traditional assistive technology devices for various tasks. There are apps available that can identify objects, assist with navigation, and even connect users with volunteers who can provide remote assistance with tasks like shopping. Additionally, smartphones are used for listening to books, recognizing letters, and magnifying text. As demonstrated with my phone in a 3D-printed magnifier holder (Figure 8), magnification apps allow for hands-free viewing by simply placing the phone on the desired object and moving it around as needed.

Figure 8. Smartphone magnifier holder.
Magnifiers are available in various forms, including handheld devices or wearable versions. For some individuals, using a smartphone as a magnifier suffices, while others may require specialized interventions with precise magnification levels and training. The appropriate solution just depends on the amount of low vision a person has. Additionally, tablets and e-readers like Kindles have been beneficial for reading, with many users reporting significant improvements in their reading ability when using these devices.
Communication Devices
Environmental. When considering communication devices, environmental modifications can be implemented to improve visibility and usability. Task lighting, such as lamps placed around the device, can improve visibility and help distinguish the device from its surroundings. Increasing the brightness of the area with higher lumens or changing light bulbs can also help with visibility. Additionally, increasing the contrast between the surface and the device can improve identification. For example, using a contrasting case, such as a black device in a white case, or adding tape around the edges can make the device more distinguishable on surfaces with similar colors.
Device-based. When examining the device itself, accessibility settings offer various options to enhance usability. Adjustments such as increasing font or icon sizes, rearranging apps and grid sizes for improved scanning, and enhancing contrast settings can all contribute to a more accessible interface. Additionally, utilizing a nightlight option to soften the light color can be beneficial, particularly for reducing the disruptive effects of blue light on circadian rhythms. This feature is commonly found on computers and can be set to activate automatically at night, though some users may choose to enable it permanently to mitigate blue light exposure.
Furthermore, another useful feature is the ability to reduce the white point, a function available on iOS devices and through various apps on Android. This feature softens the contrast of white elements on the screen, reducing the sharpness that can cause discomfort. Many users, including myself and numerous clients, have found this adjustment to be highly beneficial for enhancing comfort during device usage. Additionally, accessibility options such as reducing motion effects when navigating through apps can further improve the user experience. And, of course, adjusting the screen's brightness, while important for visibility, requires finding the optimal balance to avoid straining the eyes.
Additionally, it's worth noting ongoing research efforts aimed at developing video enhancement technology to improve the readability of facial expressions during video calls for individuals with low vision. While promising, this technology remains primarily within the realm of research and hasn't yet transitioned into widespread practical applications.
Figure 9 shows screenshots from a device we used at work. As you can see, we have the option to adjust the brightness and grid alignments. Apps can be positioned in the center, right, or left, and their sizes can be modified according to individual preferences. Additionally, one of the folders is displayed in a different color for improved contrast compared to the white background. In some cases, the colors can be inverted, displaying a black screen with white text or vice versa. These accessibility settings can be customized to meet the specific needs and preferences of users. Similar adjustments can also be made on computers using various control devices to enhance accessibility further.

Figure 9. Device screen options.
Case Study
Let's look at a case study from my experience working with a client named Edna. I was part of a program called CAPABLE, which is affiliated with Johns Hopkins and involves occupational therapy (OT) and nursing interventions. In this program, I had six visits with Edna, while my nursing colleague had four visits. Additionally, a handyman was involved to carry out home modifications and repairs as needed. During our sessions, Edna and I collaborated to establish goals using a coaching approach, which differs slightly from traditional OT methods.
Edna, aged 69, lived independently and was retired. She received daily visits from her daughter, who brought along her young grandchildren—a two-year-old toddler and a baby. Edna had a complex vision history. She had a stroke with a brain aneurysm along with right eye blindness, floaters, flashers, cataracts, macular degeneration, glaucoma, and general low acuity. Despite her visual challenges, she enjoyed activities such as watching TV, reading, crafting, talking on the phone, and spending time with her grandchildren.
Edna resided in a three-story row home in North Philadelphia, reflecting the urban environment where I live and work. Her home lacked sufficient lighting, with many light bulbs missing or extremely dim. During an assessment, I measured the ambient light, reaching a maximum of about 1000 lumens when standing near her staircase directly beneath a light fixture, with all lights turned on.
The overall lighting situation in Edna's home was notably dim, measuring around 1000 lumens in the brightest areas, significantly lower than the typical minimum of around 3000 lumens in most homes. Moreover, there were multiple areas with low contrast, including a step leading to another room and the dimly lit corner where she kept her communication and reading tools. This setup made it challenging for her to navigate and access these devices, even when sitting in her recliner chair. Consequently, she struggled with tasks such as reading, using her phone, and managing her computer for social media and bill payments, exacerbating her already difficult vision situation.
Interventions for Low Vision
To address the lighting issues in Edna's home, we took several steps. First, I upgraded all the light bulbs to maximize the available lumens without overloading the fixtures. Additionally, I installed extra puck lights throughout the space to further enhance the overall brightness.
I also provided Edna with instructions on how to clean the glass fixture covers to improve light transmission. Despite encountering resistance from the handyman, who was hesitant to tackle the task due to the height of the ceilings, I advised Edna to soak the covers in hot water and vinegar for 24 hours to remove any accumulated cigarette tar. Fortunately, she had someone coming to clean her windows who could assist with this.
In addition to these measures, I introduced a new task lamp specifically tailored to Edna's needs. This lamp offered adjustable settings for both lumens and kelvins, providing flexibility to adapt the lighting according to her preferences. Although I initially considered smart light bulbs, I ultimately opted for a more straightforward solution to meet her immediate needs.
Considering Edna's apprehension with technology and her preference for simplicity, I focused on enhancing her task lighting using conventional methods rather than relying on smart technology. I relocated her devices closer to her favored chair and implemented a revised organizational system to ensure easy access while also maximizing the contrast between her storage areas and devices so she could see them.
As you can imagine, there were numerous modifications that happened related to reducing her risk of falls. Given Edna's extensive low vision history and the need for significant magnification, I opted for a hands-free magnifier that rests on her chest and is worn over her head. This choice allowed her to work with her hands freely while maintaining close proximity to the magnifier for reading and other tasks. While there are various types of magnifiers available, this particular model suited her needs best.
Next, we tackled the accessibility settings on her computer. After adjusting the screen brightness to a more comfortable level, we activated the nightlight feature to soften the color for her eyes. Increasing the font size across the entire computer interface was another adjustment made through accessibility settings. Additionally, we enhanced the visibility of the mouse pointer by enlarging it and changing its color to bright green, making it easier for her to locate and navigate on the screen. For her Kindle reading device, we adjusted the font size and line spacing to better suit her needs. Fortunately, her Kindle had a matte finish, reducing concerns about glare and enhancing readability.
Regarding her outcomes, one of Edna's primary goals was to feel safer in her home and reduce the risk of falls. Since implementing the modifications and improving the lighting, she reported feeling significantly safer and experienced fewer falls. She effectively utilized her adaptive equipment and task lighting to navigate her environment with more confidence. It's important to note that achieving these outcomes required both environmental modifications and behavioral interventions. Through collaborative decision-making and comprehensive training, we tailored solutions to suit her specific needs and preferences.
Her active involvement in decision-making significantly contributed to her adherence to the interventions. By providing client education and allowing her to make choices, we fostered excellent carryover for fall prevention and device utilization. One of her key goals was to manage her bills more effectively. She was struggling to read them and, as a result, was falling behind in her payments. With improved vision, she regained the ability to read and track her bills, resulting in timely payments. Additionally, she resumed participating in leisure activities and communicating with her family and friends more easily. We also contributed to some of these cognitive organization strategies because she actually could see her environment much better to be able to use them.
Summary
In conclusion, as more individuals opt to age in place, it's imperative to tailor environmental modifications to address specific challenges related to vision impairment. These modifications should prioritize aspects such as lighting, glare reduction, contrast enhancement, and minimizing visual distractions while also supporting existing compensatory strategies. Employing a diverse range of intervention approaches tailored to each individual's needs yields the most effective outcomes. Integrating assistive technology with behavioral interventions and environmental modifications enhances overall effectiveness. Furthermore, exploring the built-in accessibility features of existing devices can uncover valuable tools to improve accessibility for individuals with vision impairments.
(I want to thank my colleague and SLP, Lindsay Milgram, who assisted me in making sure this content is accurate and supportive of communication.)
Questions and Answers
I'm a little confused about light bulbs. Do lower kelvins or lumens equal warmer or yellow light?
The lower Kelvins equal the warmer light; lumens just mean that it's brighter. You just have more. It's like the difference between high noon and evening. Kelvins are the color. A lower Kelvin number provides a warmer, more yellow light.
Do you recommend the use of assistive devices like Alexa?
There's actually a lot of really interesting literature on those speaker systems in terms of how they work, how they support cognition, or if they work well in different homes. So, for the right person, it can be really helpful if someone's familiar with the technology, if they're able to remember the commands, and if it works well in the home because of acoustics. It is something that can be helpful for the right person.
Is there any way to make screens more matte?
Yes, you can actually buy different screen protectors online. I often see them in the design field to give people a more paper-like feel when drawing on their tablets. You can also just buy covers. I have blue light blockers and screen protectors on my external monitors right now, and then you just put them on like a film.
I have a patient very similar to Edna. She wants to remember to take her meds while alone.
I would look into smart devices that have auditory reminders - those are typically helpful for individuals. I've also used different size signs that they can read. Or you can try to get them into a routine. There are many different ways you can approach that. But the smart device would be something that I would ask if the person's comfortable with and then go from there.
What are some good resources for practitioners if they want more information on these amazing topics you covered?
I know that there are some universities that do different low vision certificates that can be useful and very interesting for further advanced study. In terms of smart technology, at least in OT, there's always a conference presentation or poster on this topic. But they change so fast that sometimes the best thing to do is go to the store and play with them yourself because tomorrow, there could be a new device available. I actually follow many social media accounts where people spend their time looking at devices and strategies. That's actually where I have seen some pretty cool ideas.
In terms of home modification, there are different certifications that do exist. You see two of them in my credentials, and there are many online programs that you can take that would get you a certification as well.
References - See handout for a full list of references
Citation
Chabot, M. (2024). Environmental modifications for adults with low vision. SpeechPathology.com. Article 20658. Available at www.speechpathology.com