Editor’s note: This text-based course is an edited transcript of the webinar, Caring for Yourself While Caring for Others, presented by Kathy Pillow-Price, EdD.
Learning Outcomes
After this course, participants will be able to:
- Define burnout, vicarious trauma, compassion fatigue, and secondary trauma and examine how they can be prevented.
- Identify and highlight protective factors and self-care strategies that can be implemented by individuals and organizations.
- Identify the roles managers and organizations have in preventing burnout, vicarious trauma and secondary trauma by building trauma resiliency.
Welcome
Before we begin, I would like to disclose that in this training we will discuss trauma. I want to make you aware of that upfront in case you know that you are easily triggered.
If you were to get to know me, one of the things you would learn is that I am a huge fan of Mr. Rogers. I watched his show, Mister Rogers’ Neighborhood, when I was little, I can sing all the songs, and I have studied him as an adult interested in child development. I love this quote by him that says, "Anyone who does anything to help a child in his life is a hero to me." Mr. Rogers would call you a hero because of the work that you do every day. I want you to know that I do too.
Here is another quote from Mr. Rogers that I like that talks about looking for helpers. “When I was a boy and I would see scary things in the news, my mother would say to me, ‘Look for the helpers. You will always find people who are helping.’” Those in the early childhood field often notice that there are close relationships between people who are helpers and those that they help. Many helpers enjoy positive feelings that come from building trusting relationships with families and seeing improvement as a result of those relationships. However, many families are living with the impact of things like trauma, death, violence, fear, poverty, depression, hopelessness, helplessness, and other physical and mental health issues. As a result of these relationships, helpers are exposed to the distress and pain experienced by families and their young children. Dealing with families who suffer is draining and it is a difficult aspect of our work. As a result, the question is not whether stress will appear as a result of exposure, but to what extent.
Definitions
Burnout, vicarious trauma, secondary traumatic stress, and compassion fatigue are some of the words you use to describe what helpers can feel. Let's take a look at what they mean.
Vicarious trauma is the emotional duress that results when an individual experiences trauma through hearing the stories and observations of another. John Ortberg is an author and speaker that I liked and he says there are two types of suffering. There is suffering from and suffering with. Vicarious trauma is when we suffer with someone. Suffering with is voluntary suffering. We stop what we are doing. We sit beside a bedside or we listen to a mom that has lost her child. We bring meals to a family that has lost a loved one. In these acts, there is a transfer of burden as we sit with others. Vicarious trauma occurs when we suffer with someone and it hurts almost as much as a suffering from it ourselves.
Secondary traumatic stress is a secondary trauma which results from indirect exposure to trauma. It was defined by Dr. Charles Figley in 1995. He said that secondary traumatic stress disorder is the reaction a person has when they hear stories or experience trauma vicariously through indirect exposure and leads to PTSD symptoms. The stress results from helping or wanting to help a traumatized or suffering person.
Compassion fatigue is a less stigmatizing way to describe secondary traumatic stress. Trauma is not experienced as a victim but through secondary exposure to a victim’s story or experience. Compassion fatigue can lead to post-traumatic stress disorder (PTSD) symptoms. PTSD is a primary trauma which results from direct exposure to the traumatic experience. What we know though is that symptoms of primary and secondary trauma can be very similar.
The last thing we are going to look at is burnout. Burnout is a severe state of exhaustion or lack of energy that is usually brought on by unreasonable work expectations or from other work-related stress. Although burnout has many of the same causes and symptoms of secondary trauma, burnout results from long-term non-supportive work environments. It differs from secondary trauma in that exposure to clients' trauma is not the precipitating factor. People suffering from burnout may also suffer from compassion fatigue. However, the cause of burnout is more related to external working conditions.
Compassion Fatigue
While it is not uncommon to hear compassion fatigue referred to as burnout, the conditions are not the same. Compassion fatigue is more treatable than burnout, but it can also be less predictable and may come on suddenly or without much warning whereas burnout usually develops over time.
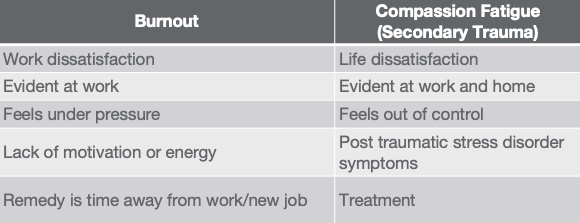
Figure 1. Comparison of burnout and compassion fatigue.
As you can see in figure 1, burnout is when you are dissatisfied with work, and compassion fatigue is life dissatisfaction. With burnout, you feel under pressure, and with compassion fatigue, you may feel out of control. With burnout, taking time away from work or getting a new job will often fix the problem, but compassion fatigue requires a different treatment.
In the words of the founder of compassion fatigue, Dr. Charles Figley, "Compassion fatigue is a state experienced by those helping people or animals in distress. It is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create a secondary traumatic stress for the helper."
Risks
So how do you know if you are at risk? Compassion fatigue is a serious occupational hazard for those in any kind of helping profession. The majority of those in a helping field report that they have experienced at least some degree of it in their lives and 50% report that they are currently experiencing some symptoms. Any professional who works directly with traumatized children and their families and hear stories of traumatic experiences is at risk for secondary traumatic stress or compassion fatigue. Typically, those with the most empathy are the ones that are most at risk.
Signs/Symptoms
Compassion fatigue symptoms will show up in multiple areas of your life including physical, psychological, emotional, spiritual, personal, and professional, as seen in the list below.
- Fatigue or illness
- Cynicism
- Irritability
- Reduced productivity
- Feelings of hopelessness, anger, despair, or sadness
- Anxiety
- Appetite changes
- Feeling overwhelmed
- Feelings of re-experiencing an event
- Sleep disturbances and nightmares
- Avoidance of people or activities
- Persistent anger and sadness
- Poor self-care
It includes things like chronic exhaustion which can be emotional, physical, or both. It also includes things like reduced feelings of sympathy or empathy and feelings of irritability, anger, or anxiety. There are physical symptoms like headaches, trouble sleeping, weight loss, impaired decision-making, problems in personal relationships, and poor work-life balance. Notice as you look at the list above how they cross boundaries of mind, body, spirit, and emotions. Compassion fatigue affects you as a whole person.
This is a good place for us to pause for a few minutes and reflect. I would like for you to write one or more symptoms of compassion fatigue that you have experienced. Figure 2 shows a list of symptoms from Dr. Figley for you to look at as you are writing. Take a moment to review these and reflect on then write down any that you have personally experienced.
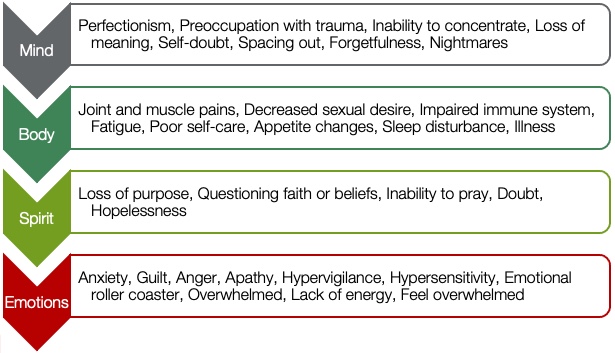
Figure 2. Symptoms of compassion fatigue.
If we were doing this training in person, I would ask you to hold up your list forward-facing and walk around the room and read how compassion fatigue is affecting not only you but also your coworkers and your colleagues. Every time that I have done this with a group, I can tell that there are those who probably do not want to share their symptoms. I always take the time to thank them for having the courage to share with others. I want to thank you today for having the courage to reflect on what is currently going on with yourself.
What I hope when I do this exercise after participants walk around a training room and they start to see heads nod, is that they will know that they are not alone, and you are not alone either. You are not alone. I ask you to do this reflection because the prevention of compassion fatigue starts with awareness. We must understand that we are at risk to get to the scope of this issue.
Personal Story
You have completed some reflecting on your own story. Now I will share a little more about my story and the reason I am so passionate about sharing information on caring for yourself. I have always loved stories of strong women, perhaps because I have been blessed with them on both sides of my family. The foundation has always been my mom and her three sisters. Through good times and bad, through success and failure, they have always been there for me. My mom and my aunts taught me to live life with joy.
A couple of years ago, when I celebrated one of those milestone birthdays, my mom and aunts were there when my handsome, wonderful husband got me good with a surprise birthday party. At that party we laughed, we ate cake, we ate pizza, and we enjoyed being together. Unfortunately, it was also the last time that I would see my Aunt Vada alive.
On March 24th, 2018, she was brutally assaulted and murdered in the home that she had lived in for the past 40 years. My experiences as I have grieved her loss are why I am here today talking about the importance of knowing what trauma and compassion fatigue can do to an individual and why it is important that we practice self-care. On March 25th, 2018, my mom called me and was screaming incoherently that my cousin had found my aunt and that she had been murdered. My aunt was 79 years old. To understand what had happened to her was just something I could not even begin to wrap my mind around.
When we arrived at her house, we saw multiple law enforcement vehicles and the majority of my family was standing outside waiting for any news that they could get. My aunt's body had just been taken out and sent away for an autopsy. After some time, the police officers came outside and said they were done and that we could go into the house and clean and do whatever we needed to do.
My cousin, the one that had found her mother, started into the house. I knew that I could not let her go in alone. I also knew instinctively that I did not want my elderly mother and my other aunts to see how bad it was. As I entered the back door of the home, the first thing I saw were signs of struggle and blood. There was so much blood. We were advised by officials to wear gloves. I found some old kitchen towels and cleaning spray. I wet a towel and began to wipe the blood from the appliances, the floors, and the walls. I was cleaning hard and fast and it was making me physically sick. Every time I went to the sink to rinse my towel I sobbed as I watched her blood disappear down the drain. I thought about what her life was like in her last minutes on this earth.
I spent the next few days staying busy. I helped to take care of my family. I assisted with making arrangements for her celebration of life service. But the images of what I saw at my aunt's house will never leave me. After I came home, I began to suffer from horrible nightmares, fear, and anxiety. I am a strong person of faith, but during that time, I alternately prayed for help and screamed at God sometimes in almost the same breath. A few weeks later, I bottomed out. I called my pastor sobbing and I told him how angry I was. He reminded me of a quote that I had always loved that says the worst thing is never the last thing.
Law enforcement officers tell us that we are lucky. My aunt's killer was caught the day after he took her life. After receiving positive DNA results, he agreed to plead guilty if the death penalty was taken off the table and he was sentenced to life in prison without parole. I was in the courtroom and testified on the day that he was sentenced.
In light of all of that, you can see why self-care has become very important to me in the past few years. I began counseling and I started my way back to being okay. I have learned to say that I am healing instead of I am healed. Sometimes I say, I am healthier now or I am better now.
Six Environmental Conditions for Health and Growth
In the professional world, psychologists tell us that there are six environmental conditions that are required for health and growth. These are required for individuals, families, organizations, and sometimes even entire communities.
- Safety
- Belonging
- Consistency/Predictability
- Opportunity
- Acceptance/Love
- Hope
These are the ways that you can show up for yourself and for your peeps. When one or more of these conditions is absent or compromised, it will be difficult for a person or a group to reach their full potential. In order to prevent compassion fatigue, these conditions should be present. They should also be ingrained throughout our organizations and they should be included in our interactions with children and with families. Look at them for just a second. Are you good at all six of them? How is the organization that employs you doing with them? If you are an employer, how are you providing these conditions for your employees?
Protective Factors
Another protective factor that is important to note is that although there are risks to working in the helping field, there is also a lot of satisfaction that you can derive from your work. This is referred to as compassion satisfaction. It is defined as the pleasure and satisfaction or the positive feelings derived from working in helping caregiving systems. It is when you get to contribute to society and you help others achieve wellbeing. It is believed that compassion satisfaction is a protective factor that prevents burnout, compassion fatigue, and vicarious trauma.
People who work with trauma survivors have identified things like personal growth, spiritual connection, hope, and respect for human resiliency as positive outcomes of their work. I know when I called my pastor when I bottomed out, I apologized for calling him. I did not want to bother anyone. He said some beautiful words. He told me, “It is an honor that you have called me. It is an honor to listen to you. It is an honor to walk through this journey with you.”
Ensuring individual and organizational protective factors are in place will enhance compassion satisfaction. Here are some protective factors that organizations and individuals should have in place to prevent compassion fatigue from occurring.
Organizations
- Positive relationships within agency
- Early identification of workers dealing with stress
- Resources available for staff
- Client-centered practice
- Issues are dealt with constructively and effectively
- Communication is open and clear
- Opportunities for staff to learn and grow
Individuals
- Self-awareness
- Able to ask for help and/or get support
- Balance between home and work
- Personal strategies in place for self-care
- Open to learning and growing
- Are optimistic
- Able to set boundaries at work and home
I want you to take a look at this list and see if you can pick one thing that your organization does really well and one thing that you are doing really well as an individual in order to protect yourself. Think about these questions.
- Is your organization good with positive relationships and early identification of dealing with stress?
- Do they provide resources for their staff?
- Is communication open and clear?
- How about you as an individual? How are you doing?
- Are you self-aware?
- Are you able to ask for help and get support?
- Do you balance work and home?
- Do you have personal strategies in place for self-care?
- Are you open to learning and growing?
- How optimistic are you?
- How are your boundaries?
I share this information because I want to make it clear that everyone, including organizations, supervisors, and individuals has a role in protecting everyone from compassion fatigue.
The Professional Quality of Life Scale (ProQOL)
The Professional Quality of Life Scale, or ProQOL, is a tool that can help you determine your level of compassion satisfaction, burnout, and compassion fatigue. It is an assessment of the effects of helping others who are experiencing suffering and trauma. It has 30 questions that measure the positive and the negative aspects of caring. It is free, easy to use, and score, and you can take it as an individual or in a group. It can be taken online or there is a printable version.

Figure 3. Professional Quality of Life (ProQOL) Scale.
As individuals, the ProQOL can help you plan where to put your energy and help you increase your resilience. The ProQOL can help organizations find ways to maximize the positive aspects and reduce the negative aspects of helping. For supervisors, this can be used as information to start discussions with your employees and to personalize coaching for them.
Self-Care
What if you are not currently experiencing symptoms of compassion fatigue? It is important to remember that because of your helping role, you are at risk. I am here to remind you that you need to take care of yourself and you need to take care of each other. Watch for things in your coworkers and colleagues. While dealing with my own grief, I have done a lot of reflecting on how big the burdens are that you carry every day as you help individuals and families.
Many of the children and families that you deal with are experiencing or have experienced personal traumas. I want to remind you that if you are hearing that and listening to that, self-care for you is very important. I want you to fall in love with taking care of yourself, mind, body, and spirit. I want you to completely understand, like someone once said, that taking care of yourself does not mean me first, it means me too. I want you to be kind, be patient, be generous, and be accepting. Be all of these things to yourself. I want you to fully understand that self-care is a priority and a necessity. It is not a luxury in the work that we do.
Self-care is about being deliberate in taking time for yourself to better your mind, body, and soul. It is not about being selfish, rather it is about replenishing and refreshing your spirit in different ways.
Mental Health Self-Care Wheel
I came across the wheel seen in figure 4 which has been shared so many times that I do not really know who to give credit to, but I like it. It gives us all pause for thought.

Figure 4. Mental health self-care wheel.
Self-care is so important but we do not always think of it as a prescription for mental health. If you went to the doctor and they wrote out a prescription and said gym membership or they put on their prescription pad, leave work at work, we might actually pay attention.
Compassion fatigue crosses all dimensions of our life, spirit, body, mind, and emotions. Our self-care also has to cross all dimensions of our life. Taking care of our well-being is what keeps us healthy.
Take a look at the wheel in figure 4 again. Focus on one area that you know that you are already doing well. Maybe you are already good at the physical part. You eat healthily, you get regular sleep, and you exercise. Or maybe you are good with the spiritual part. You practice forgiveness, you spend time in nature, or you connect with your spiritual community. Perhaps you enjoy yoga or meditation. What is one thing you know you are doing really well?
Now, look at the wheel again. What areas of your life might need some work? Is there a spoke on this wheel that you need to focus more on? Perhaps it is a personal goal. Maybe you need to plan and set goals or spend more time with family. Perhaps you want to read more books. Whatever it is, set the goal and learn to do better at providing self-care for yourself. Can you say you are already doing a great job in all six areas? All of us probably have some room for improvement. What area can you improve in?
At the beginning of our session, I asked you to list one or more symptoms of compassion fatigue that you are experiencing. Now, I would like for you to take a moment and list one or more of your favorite forms of self-care. Perhaps you will consider writing a goal that you will practice today or this week.
If we were in person just as before, I had the participants walk around and have a check-in time in order to learn from each other. We would do that again here in order to find how others practice self-care. It is great to learn from other people.
Types of Self-Care
Figure 5 shows some of the different types of self-care frequently mentioned in the check-ins.

Figure 5. Types and examples of self-care.
Are there any that you would add? Are you good at all of these? Physically, are you getting enough sleep? Are you stretching and walking? Are you eating healthy food, doing yoga, and getting enough rest?
How about emotionally? Are you practicing stress management? Are you forgiving? Are you compassionate? Are you kind? What about socially? Do you know how to set appropriate boundaries? Do you have a support system in place? Can you communicate? Can you ask for help?
Then the spiritual dimension. Do you have time alone, whether that is time to meditate, do yoga, connect with nature or journal? Where is your sacred space? Are there any of these forms of self-care that you should consider adopting? Are there any that you should write a goal for?
After my aunt’s death, I learned that the trauma of that shocking loss caused my brain to be hijacked. It slowed my prefrontal cortex where regulation, decision-making, and problem-solving are located. This past couple of years, I have really had to ramp up my personal self-care. I have had to be more intentional in order to take care of my body, my mind, my spirit, and my emotions.
One-Word Challenge
Every year, I do the one-word challenge. Most years my words are very active and ambitious. In the past, I have chosen words like courage, all in, and finish. But the year preceding my aunt's death, I chose a different word. My one word that year was rest, as I had to purposefully make rest a high priority in my life. That is not easy for me. You see, I am a doer by nature. I even have a sign that sits on my desk that says, make things happen.
But I hit a wall shortly after my aunt's passing where I had to rest. In fact, there was one weekend where I slept 36 out of 48 hours. I was not sick and I was not tired. I was weary and my soul was weary. I had to recognize that I could not keep the pace in which I normally ran my life. So now, I have reverted back to what I was good at in kindergarten. I nap and I take pauses during the day. At night if I am tired, I go to bed. I got serious about saying no to commitments and not over-scheduling myself. I take a lunch break, I read, I rest, and I refuse to be hectic.
Take Five Breathing Breaks
One of the other things that I have done for my personal self-care is I started practicing take five breathing breaks. Take five breathing is a wonderful way to switch off the stress response. It brings the body back into balance, slowing and deepening the breath and slowing down the heart rate while harnessing the need to move with an action that requires focus and provides sensory feedback to the brain.

Figure 6. Example of take five breathing exercise.
Figure 6 shows what that looks like. Spread your hand out and stretch it out like a star. You can choose your left hand or your right hand, it does not matter. Now pretend the pointer finger on your other hand is a pencil. Imagine just like when you were a child that you are tracing the outline of your hand. Start at the bottom of your thumb and slide your fingers up and over. Continue tracing your fingers up and down and slide your fingers slowly and notice how it feels. Keep going until you have finished all five fingers.
Now you are ready to add some breathing. Breathe in through your nose and breathe out through your mouth Remember to keep this slow and steady. Place the pointer finger at the bottom of your thumb as you start and breathe in as you slide up and breathe out as you slide down, breathe in as you slide up the second finger, and breathe out as you slide down. Keep going, slow and steady until you have finished all of the fingers. Then notice, how does your body feel now? Do you feel calm? Would you like to take another five?
There are lots and lots of different ways to practice and enhance your breathing. Take five is the one that I have enjoyed but there are a lot of apps and help that you can find. One of the things that you can do with take five breathing is add in positive sayings, meditations, or breath prayers. Look them up online. Learning to slow down and breathe has been essential for my health.
Job Change
One of the harder things that I did after my aunt passed was take a new job. For six years, I was the director of the Arkansas Home Visiting Network and I loved my work. I loved the people I worked with. Most importantly, I loved the families and the children in Arkansas that we were helping. But I worked long hours and I often felt like I had the weight of the world on my shoulders. I commuted about two hours each day and I traveled frequently. We kept expanding and I refuse to do anything halfway. Then it just felt like I no longer had the energy to give it 100%. I got a job offer and with this offer, I could work from home, I could travel less, and I could still work in my field. I could still be a helper. I made the very hard decision for me to leave a job that I loved for something that was less demanding.
Mental Health Services
Another thing that I had to do was get professional help from a counselor. I was suffering from post-traumatic stress disorder (PTSD) and from complicated grief. It was more than I could manage on my own or even with the help of supportive friends and family. I needed a professional.
Many mental health services can now be delivered online without face-to face-therapy. Choosing a therapist is a personal matter. Human connection is at the heart of effective therapy. You can build that sense of connection whether you meet your therapist in person, on the phone, or online. The cool thing about therapy is that everyone can benefit from it. Everyone has a brain, thoughts, and emotions so it is worth having a professional help you examine those thoughts to determine if all of them are healthy. This applies whether you are coping with grief, trauma, relationship issues, or you want treatment for a mental illness. Finding a helpful therapist can help you make a big difference in your own personal journey.
Closing
If you have experienced trauma yourself, or you have helped others with trauma and you are experiencing some of the symptoms of compassion fatigue, I would like to leave you with these parting thoughts. First, know that it does get better. Maybe not all at once, but eventually your hope and your satisfaction will return and you will once again love helping others. I want you to continue doing your amazing work of being a hero and being a helper. I want you to be there for others but never leave yourself behind. I want you to show up for your peeps, your colleagues, and others that are in the early childhood field. I want you to encourage them to practice self-care.
Sometimes when one of your coworkers or perhaps it is one of your employees starts to act a little different, or they appear like they are not as motivated anymore, it is worth stopping to ask what is happening. It may be that they are not lazy, they are coping. Pay attention, ask questions, notice things, and make sure people are okay. I want you to practice self-care in some way every day and ask others to do the same. Dodinsky said, “Be there for others, but never leave yourself behind.”
What are you taking away from the session? I hope you have learned how to identify and define compassion fatigue, burnout, and self-care. But now take some time to reflect, what stands out for you? What will you remember? What will you do differently because of what you have heard today?
You can my references below if you would like to do more reading. I highly recommend the first one, "When compassion hurts: Burnout, vicarious trauma and secondary trauma in prenatal and early childhood service providers." I also highly recommend the second one, "Preventing compassion fatigue: Caring for yourself" by the National Association for the Education of Young Children (NAEYC). I highly recommend that you learn more about the subject and that you continue practicing self-care on your own. Thank you for joining me today. Be well, everyone.
Questions and Answers
Many larger programs have employee assistance programs (EAP) that provide assistance and services to help when someone is going through burnout, compassion fatigue, trauma, or facing any other issues. Where can smaller programs go to get some assistance?
One of the things that I would recommend is crisis counseling. Go online and Google “free crisis counseling” as well as your state. A list of providers or a website will show up that provides those types of free resources.
Another thing is to consider going to someone like a pastor or a rabbi or a spiritual leader that has been trained in counseling but is not a mental health therapist. They can direct you towards resources, but they can also, depending on the extent of counseling that you are needing, provide that free for you or to direct you where you could get counseling based on their knowledge.
Another resource, if you cannot find it from Googling free crisis counseling or going through a faith-based option, is to look at colleges and universities. A lot of them that have counseling and psychology programs also have free clinics on their campus. They are either free or low-cost. You are talking with a student that is preparing to go in the field but they are about to graduate and be a licensed therapist. You get the benefit of not having to pay for the knowledge that they are getting in school.
Let me say also to take advantage of those EAP programs. That is exactly what I did when I went through my trauma. I was very lucky that my employer provided me with free services that I used and needed. I had never even heard the term complicated grief until I went to therapy.
You talked about the ProQOL, which can be found at proqol.org. I know they have a lot of additional resources and things that you can do. Are there any websites or apps that stand out to you that might be helpful?
I am a podcast and an app person myself and do not do as many website searches. Look for apps that promote self-care, breathing, mindfulness, and meditation. Do those types of searches and find the ones that work for you. I did the take five breathing because it is something that can ground me immediately and physically.
I also do mindfulness training every day on my Fitbit. I have that as a goal that I do that at least five times a week and my Fitbit keeps up with it. I just go in there and find the mindfulness training that I want to do for that day. Everybody is a little different in what they want. I usually tend to look for things that not only take care of me but advanced my faith. Some people do not want that part, they want the more meditative things.
How would you recommend approaching a person that is starting to show some signs of compassion fatigue, whether they are a colleague or an employee?
One of the things that I would make sure you do is approach them in private. Make sure it is very conversational and comes from a place of concern, care, and support. Ask them, how are you doing? Tell them you care and would like to know how they are doing. If they open up and share, great. If they do not, keep asking a few open-ended questions or make statements such as, I have noticed a few changes and I just want to make sure that you are okay.
When I was the director of the Arkansas Home Visiting Network, we had wonderful EAP services and I would keep the cards for it in my desk. There were a couple of times that I would take a card out of my desk and push it across to the employee and gently say, I am not a mental health professional. I am not saying that you need this. I am telling you that I have done this. If you have any questions, I would be glad to answer them. If you want services like this, you need to know that we provide them and that it is free and confidential. I am not going to know whether you go or not. Nobody is going to know what is said there. But you need to know that these services are available for you.
If you are in a small organization, I would look up some resources in advance. Again, just say, I am not saying you need this, I am saying that I want you to know what is available. I want you to know that I care and I have noticed changes, and I am here for you if you want to talk. One of the best things that we can provide is support and listening. In one of my communities we say, listen, listen, love, love. That is what people need from us as employers or as coworkers.
References
Best Start Resource Centre (2012). When compassion hurts: Burnout, vicarious trauma and secondary trauma in prenatal and early childhood service providers. Toronto, Ontario, Canada: author.
Erdman, S., Colker, L., and Winter, E. (2020). Preventing compassion fatigue: Caring for yourself. Young Children, 75 (3).
Figley, C.R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel.
Figley, C. R. (Ed.). (2002). Psychosocial stress series, no. 24. Treating compassion fatigue. Brunner-Routledge.
National Child Traumatic Stress Network, Secondary Traumatic Stress Committee (2011). Secondary traumatic stress: A fact sheet for child-serving professionals. Los Angeles, CA, and Durham, NC: National Center for Child Traumatic Stress.
Ortlepp, K., & Friedman, M. (2002). Prevalence and correlates of secondary traumatic stress in workplace lay trauma counselors. Journal of Traumatic Stress, 15, 213-222. doi:10.1023/A:1015203327767
Siegfried, C. B. (2008). Child welfare work and secondary traumatic stress. Child Welfare Trauma Training Toolkit: Secondary Traumatic Stress. The National Child Traumatic Stress Network. Module 6, Activity 6c.
Stamm, B. H. (Ed.) (1999). Secondary traumatic stress: Self-care issues for clinicians, researchers, and educators (2nd ed.). Washington, DC: Sidran Press.
Citation
Pillow-Price, K. (2021). Caring for yourself while caring for others. Continued.com - Early Childhood Education, Article 23725. Available at www.continued.com/early-childhood-education

