Editor’s Note: This text is a transcript of the course, ALS: Impact on Nutrition, presented by Denise Dougherty, MA, SLP.
Learning Outcomes
After this course, readers will be able to:
- Describe the impact of ALS on nutrition.
- Explain the rationale for PEG placement in the patient with ALS.
- Identify three strategies to improve nutrition
Introduction and Overview
In Part 3 of this series, we are going to talk about the impact of nutrition in amyotrophic lateral sclerosis (ALS). Let’s first briefly review what was discussed in the past two sessions. Part 1 dealt with medications and oral care, and in addition to that, we looked at supplements and vitamins, including creatine and vitamin E. I received a study within the last couple of days that contains a bit of new information, and I would like to pass that along. This study suggested that ultra-high doses of vitamin B12 given within one year or less of symptom onset caused improvement. In Part 2, we discussed therapeutic exercise, specifically looking at tongue strengthening and respiratory exercise. We talked about the breather and expiratory muscle strength training (EMST), tools that are sometimes a bit difficult for our clients to use. I suggested that you start with party horns, and then move up; sometimes that is the “baby step” that the patient needs. We discussed the treadmill and swimming for overall body exercise, and another study just came out that suggested improvement in muscle function with swimming.
In this course, we will review the nutrition factor, look at diet recommendations and the pros and cons of percutaneous endoscopic gastrostomy (PEG) tube use. After this course, you should be able to explain the impact of ALS on nutrition, discuss the rationale for PEG placement in the ALS patient, and identify at least three strategies to improve nutrition.
It is important, when we work with this population, to be very aware of the impact of the disease on nutrition. There will likely be a need to modify the diet and look at strategies, and eventually, we will need to discuss a PEG with this individual. Nutrition recommendations must be patient-specific because things vary from patient to patient. When we approach the individual and family about the PEG tube option, it is very important to understand that the patient and family’s culture and religion can influence their acceptance of that recommendation. As professionals, we need to be very sensitive to those belief systems, and I will have some references related to that as we go through this course.
As the individual begins to lose his or her function, it is important to talk about advance directives. That should be addressed very early on because the patient needs to tell us how nutrition should be handled (e.g., are they interested in intravenous (IV) or PEG tubes, or would they rather just continue to eat by mouth? That certainly is their choice, but we want it to be an informed, educated decision.
Nutrition
Psychological and Physical Well-Being
When talking about life expectancy, we have to understand how important psychological well-being is. Individuals who are more positive tend to have an improved life expectancy.
Nutrition plays a big role in that as well. We will have to investigate and discuss the use of enteral nutrition. Because our patients and their families have limited information about the PEG, they sometimes want to push that decision off until later. However, the problem with ALS is that there is a window of opportunity where there is a better survival rate. If it is discussed or placed too late, it could increase the individual's chance of death during that procedure. Therefore, we have to talk about it very early. Patients need to prepare themselves.
Certainly, nutrition is a major issue with neurodegenerative diseases. More than half of speech pathologists report that patients do not adhere to strict enteral nutrition. The major factors that tend to influence that adherence would be diarrhea and increased reliance on caregivers. There is often the option of a hybrid type of approach, where the patient can still consume food by mouth, but we provide the calories or hydration they did not take in orally, via the feeding tube. Sometimes insurance companies make it a bit sticky, so it is just an education process for our patients. I know that my clients, no matter what the disease process is, are just more likely to continue eating by mouth. It is what it is, and that is their choice, as long as it has been an informed, educated decision.
Nutrition worsens during the disease progression, and if nutrition is not appropriate and does not meet a patient’s needs, that is associated with higher mortality. Therefore, we need to talk about diet modifications and discuss the PEG tube issue.
Protein deficiency - protein malnutrition - is often found in these individuals. If you do not consume enough protein, it causes problems with gas exchange because intercostal muscles do not work well. That can create respiratory failure and death.
ALS Association Resources
These are some articles related to nutrition that can be found at the ALS Association:
- Safe Swallowing: What I Need to Know and Why it Matters
- Adjusting to Swallowing Changes and Nutritional Management in ALS
- FYI Feeding Tubes
- PEGS and Nutrition in People with ALS
There are a number of handouts and resources at the ALS Association, but these specific articles will help your patients and families understand the changes that will occur with nutrition. The more information we can give them in writing the better; so that they can always go back and review it at their leisure. When we educate them during a session, there is only so much information they can take in. They are dealing with so many issues. They remember bits and pieces, but not the entire conversation. Sometimes they change the content in their minds; it is not what we said, but in their minds, that is what they heard. So the more we can give them in writing, and direct them to different support systems such as these different associations, the better it is.
Taste
Everyone begins to lose their ability to taste and smell as they age. That is very debilitating. Loss of the sense of taste is a common feature in ALS. It can be a combination of the disease process plus medications plus the impact of aging. That loss of taste changes the perception you have of food in the mouth. When you put food in your mouth, it initiates many different responses. There are mechanical and chemical stimuli that send messages to the brain.
Anytime there is an impairment in any of the systems (oropharyngeal, esophageal, etc.), it can compromise gastrointestinal functions. Therefore, taste is often a huge issue for individuals with ALS. We may be able to add spices, herbs, and flavonoids to enhance flavor. Monosodium glutamate (MSG) is an example of a flavonoid we can add to the foods.
Taste is a critical factor for our patients. Many times they say that everything tastes the same or food has no taste. That impacts their oral intake.
As we begin to change our patients’ diets and modify the consistency of the food, chewing can become unnecessary for them. Unfortunately, it is that chewing action that actually helps release the flavor in the food. The less they have to chew, the less that flavor is available to them.
Sensory changes, not just from the disease process, but also due to aging, impacts quality of life. Even patients who have PEG tubes placed talk about the severe loss of taste perception. If they are strictly nothing by mouth (NPO), that is one thing, but if they are doing the hybrid approach and are eating by mouth as well as using the feeding tube, that is going to be a real issue for them.
There is a device that has had some clinical trials. It actually provides flavors of natural meals. You apply this device on the tongue for 20 seconds and it allows you to perceive flavors of the food without having to swallow. This is still in the testing stages. There is an article about it by Tarlarini et al. (2018) in the references list if you want to read about this study. I thought it was an interesting way to provide the flavors without actually giving them the food.
Optimizing Nutrition
It is really important that nutrition is optimal for these individuals because it helps them survive for a longer period of time. Survival is also better if we have more albumin in our system. One of the factors that is often looked at before a PEG tube is placed is the level of albumin in the system. The research shows that there is a link between low albumin levels pre-PEG, and a high mortality rate after the PEG is placed. So, in addition to the dysphagia and the respiratory issues related to ALS, they may also look at the levels of albumin. You may find that information in the doctor's discussion of whether it is a good time to place the tube, and whether it is a good strategy for the individual.
The earlier we get involved with individuals with ALS, the better chance we have to optimize nutrition. Evidence suggests nutritional therapy needs to start almost at the time of diagnosis so we can slow down that decline and help patients with strategies.
Muscle Atrophy, Weight Loss and Body Mass Index (BMI)
Muscle atrophy is very characteristic of progressive diseases. The individual is fatigued and does not do a lot of moving, which then increases the muscle atrophy. In addition, they are using a lot of energy just in the process of breathing, so that is an issue.
There is a direct association between weight loss and disease severity. At the time of diagnosis, a 5% reduction from normal weight actually increased the risk of death by 30%. The loss of one kilogram per meter in BMI was associated with risk of death being increased by 20%. Nutrition is really important, and we need to collaborate with the dietitians to improve that.
There is decreased muscle mass with this disease, regardless of whether there is weight loss. We see reduced muscle mass in aging as well. This includes loss of mass in the chewing muscles. The masseter loses muscle mass and density, so that creates some problems with mastication.
There is an average of approximately 12 months between when the symptoms first occur and when the diagnosis is made. It has been found that in that timeframe, about 50% of motor neurons have been lost. Part 2 discussed the rating scale, the ALS Functional Rating Scale (ALSFRS), and that is a good measure of muscle strength and lung function. Patients tend to lose fat reserves before we start to see a change in body weight. Then there is a downward spiral that begins, where you see a decrease in what is called fat free mass (FFM) and body weight. When that decrease starts to kick in, it compromises the strength of the respiratory muscles, and therefore, the patient has to recruit other muscles to help with the process of respiration. That increases the energy requirements and expenditure, and that, in turn, increases the functional impairment. This downward spiral is shown in Figure 1.
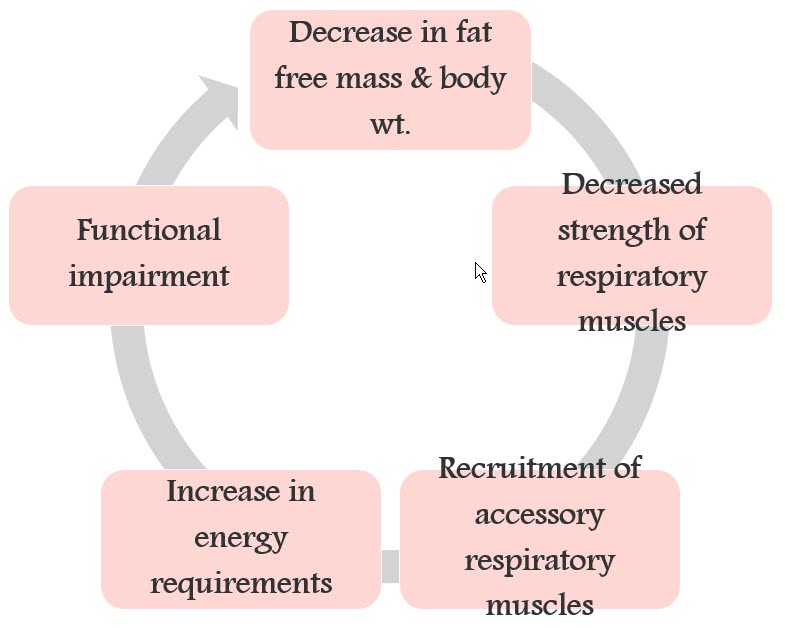
Figure 1. Impact of decreased fat-free mass and body weight on respiratory muscle strength.
Figure 2 shows another spiral. Because of the decreased fat-free mass and body weight, there is a decrease in peripheral muscle strength. This causes the individual to be less active, and that is bad news because the decrease in activity creates disuse atrophy in the muscles. Referring back to the topic of full-body exercise, the more we can keep these muscles working, the better it is for the individual’s chance of survival. Once disuse atrophy of the muscles sets in, it increases the functional impairment and we see that downward spiral again.
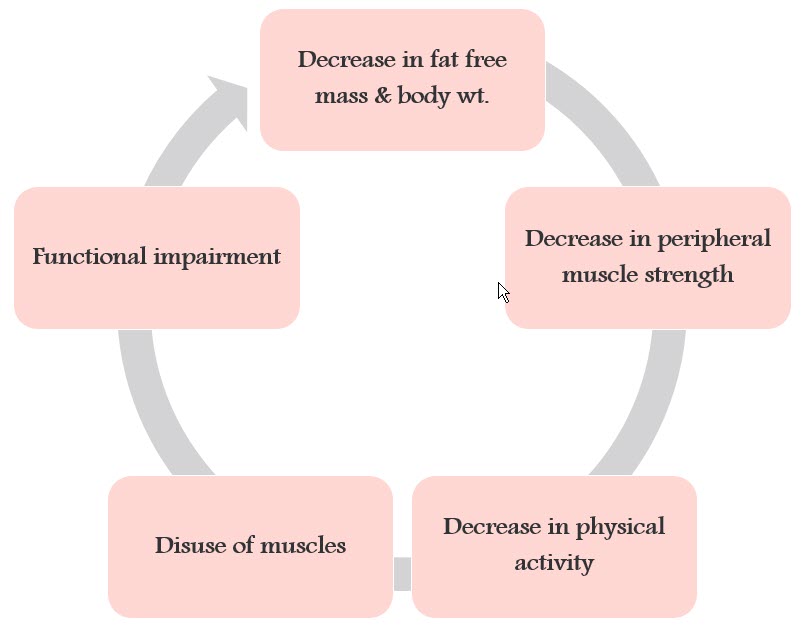
Figure 2. Impact of decreased fat-free mass and body weight on peripheral muscle strength.
Weight Gain
There has been some discussion about whether or not ALS patients should try to gain weight. It has been found that fat-free mass is actually a better predictor of nutritional requirements - better than looking at the BMI or body weight. You may work with the dietitian to get that information. A low FFM is related to increased hospital stays and mortality. Reduced energy intake often contributes to FFM depletion and also creates burdens on respiration. That respiratory burden can be reversed to some extent by the use of non-invasive ventilation (i.e., CPAP and BiPAP). On the other hand, if you gain weight, that tends to impact your inspiratory muscle functions. There is an increased likelihood of obstructive sleep apneas, a greater burden placed on inspiratory muscles, and an increased risk for nocturnal hypoventilation. So there is a fine line to walk when it comes to weight gain. We certainly do not want weight loss, but weight gain can be detrimental as well (Figure 3).
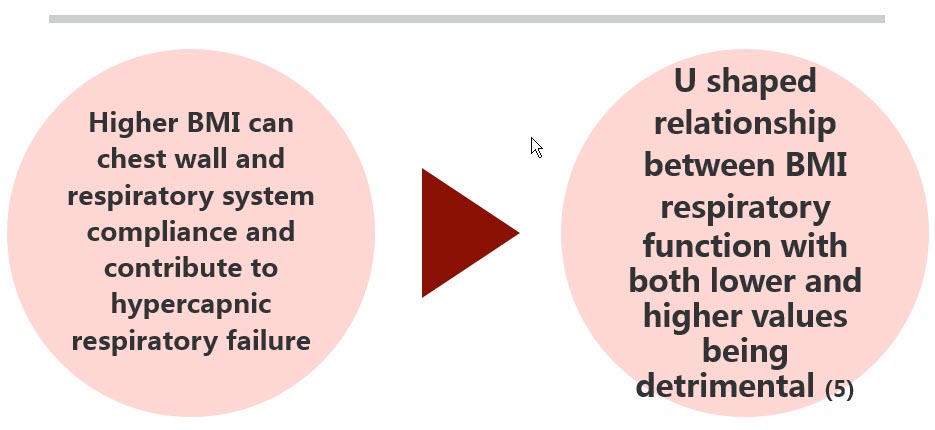
Figure 3. Impact of weight gain on respiration.
Weight Loss, Dysphagia and Supplements
It is important to increase the use of high-calorie supplements. The problem is that it is very difficult for individuals to utilize these. They often do not like the taste. You can build up a metallic taste on the tongue from the calcium salts and the other ingredients in the supplements.
We don’t fully understand weight loss in ALS. It may not be due to a dysphagia, but there is increased use of muscle energy with those muscle fasciculations and respiratory effort, and there is frequently depression, which then decreases the amount of food our patients consume. The more high-calorie supplements we can get into the individual, the better it is for them, and this should be considered very early on.
We should also discuss the PEG tube. It is the patient's choice about whether to go that route or not, but again, it should be an informed, educated decision.
There are some articles on what are called nutraceuticals. The literature suggests nutraceuticals are used by about 80% of individuals with ALS. They are self-medicating with foods, functional foods, and dietary supplements.
We need to be careful about dietary supplements because they may not work very well with traditional medications. But it’s important to recognize that our patients may be going down that road. I always want to tell my patients, “No judgment. I just need to know what you are consuming. It will be helpful to know that in case there is a potential side effect we need to watch for.”
It has been found that only about 1/3 of individuals actually use the high-calorie nutritional supplements because they are not covered by health insurance. Our patients are financially strapped and they just don’t have the money for these things. The thickener is also expensive for patients, so as much as we would like them to consume that, it may not work for their budgets.

